A Patient’s Story
When Sarah noticed a painful ulcer on her tongue, she initially dismissed it as stress or a minor bite. But over a few weeks, more sores appeared, and she also experienced heartburn and occasional difficulty swallowing. Concerned, she visited her GP, who suggested a consultation with a gastroenterologist.
At LSDC, a thorough evaluation revealed that her recurrent mouth ulcers were linked to acid reflux and an underlying upper gastrointestinal condition. Understanding the possible causes and management strategies can help others facing similar discomfort.
What Are Mouth Sores and Ulcers?
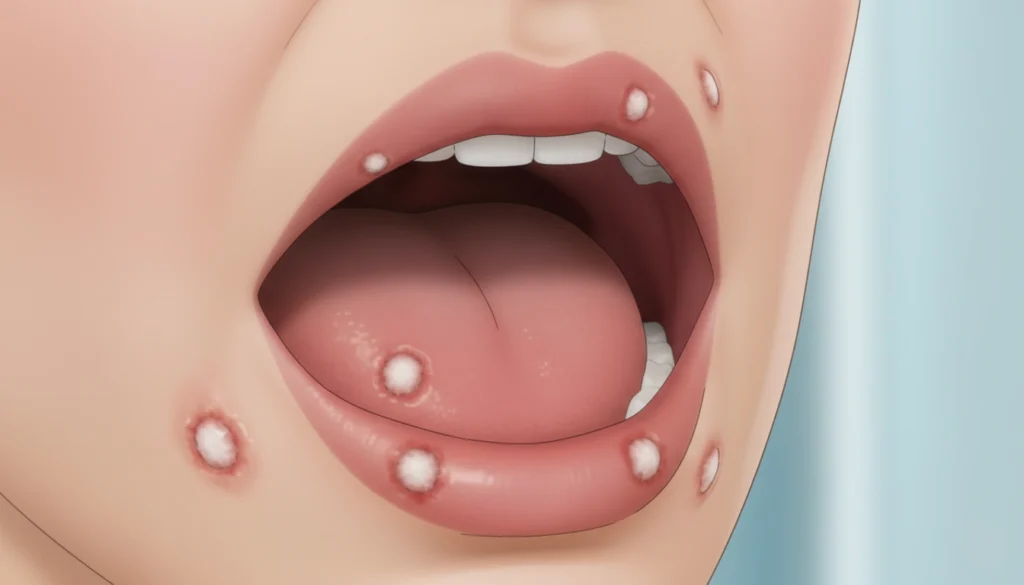
Mouth sores are painful lesions that can appear anywhere inside the mouth, including the lips, gums, tongue, cheeks, and roof or floor of the mouth. Ulcers are a specific type of sore that often presents as round or oval lesions, sometimes with a white or grey centre surrounded by redness.
While occasional mouth sores are common, frequent or recurring ulcers may indicate an underlying health issue. At LSDC, we emphasise that identifying the root cause is crucial, especially if these sores persist or occur alongside other gastrointestinal symptoms.
Common Causes of Mouth Sores
Mouth ulcers can arise from a wide variety of factors:
Minor trauma or injury: Biting the cheek or irritation from dental appliances.
Stress or hormonal changes: Emotional or physical stress can trigger recurrent ulcers.
Vitamin deficiencies: Deficiencies in folate, vitamin B12, or iron may contribute to canker sores.
Gastrointestinal conditions: Upper GI issues like acid reflux, GORD, laryngopharyngeal reflux (LPR), Barrett’s oesophagus, or oesophagitis. Lower GI conditions such as Crohn’s disease, coeliac disease, or inflammatory bowel disease can also play a role.
Symptoms That Suggest a Gastrointestinal Connection
If mouth ulcers are linked to a GI condition, you may notice additional symptoms:
Frequent acid reflux, heartburn, or indigestion
Abdominal pain or cramping
Persistent sore throat or hoarseness
Difficulty swallowing
Bloating, gas, or changes in appetite
Chronic diarrhoea or constipation
Recognising these patterns helps clinicians at LSDC determine whether further investigations are warranted.
Appearance of Mouth Ulcers
Mouth sores may vary in colour from white, grey, yellow, red, or purple. Some patterns can hint at specific causes:
White or grey ulcers with a red halo: Often aphthous ulcers, potentially linked to folate deficiency or anaemia, which can indicate coeliac disease.
Red or white persistent patches: Could signal early cancer or pre-cancerous lesions, especially if they do not heal or are accompanied by lumps in the mouth or neck.
At LSDC, we emphasise that any persistent or unexplained ulcer should be evaluated promptly.
Investigations
To determine the cause of mouth sores, a combination of clinical assessment and targeted tests may be required:
Upper GI evaluation: If acid reflux is suspected, a gastroscopy or a 96-hour pH capsule test can confirm the diagnosis.
Lower GI assessment: For suspected IBD, colonoscopy alongside blood and stool tests may be performed.
Coeliac disease testing: Blood tests and duodenal biopsy can confirm the diagnosis.
Vitamin and nutritional screening: Identifies deficiencies in iron, folate, or B12.
At LSDC, our gastroenterologists integrate these investigations with a thorough patient history to provide a precise diagnosis.
Managing Mouth Sores and Ulcers
Treatment depends on the underlying cause, severity, and frequency of ulcers.
1. Lifestyle Measures
Maintain a balanced diet rich in vitamins and minerals to prevent deficiencies.
Reduce stress through relaxation techniques, mindfulness, or gentle exercise.
Avoid irritating foods, such as acidic or spicy meals, that may aggravate sores.
Maintain good oral hygiene, but avoid aggressive brushing that can traumatise the mucosa.
2. Medications
Topical corticosteroid lozenges or gels can reduce inflammation and pain.
Anti-inflammatory mouthwashes provide relief and support healing.
PPIs or H2 blockers for reflux-related ulcers, sometimes combined with lifestyle changes.
3. Procedural Options
For refractory acid reflux causing recurrent ulcers, anti-reflux surgery or endoscopic procedures may be considered.
Nutritional supplementation may be recommended if vitamin deficiencies are identified.
Important Tips
Never squeeze or pick at sores, as this can worsen pain or cause scarring.
Track the timing, frequency, and triggers of ulcers to assist your clinician in pinpointing the cause.
At LSDC, we provide personalised treatment plans that integrate these approaches to manage both the sores and any underlying GI conditions effectively.
