LINX Procedure: Minimally Invasive Relief for Reflux
Gastroenterology
LINX Procedure: Minimally Invasive Relief for Reflux
Offering relief by reinforcing the lower esophageal sphincter (LES), this procedure stands out for its effectiveness and reduced invasiveness.
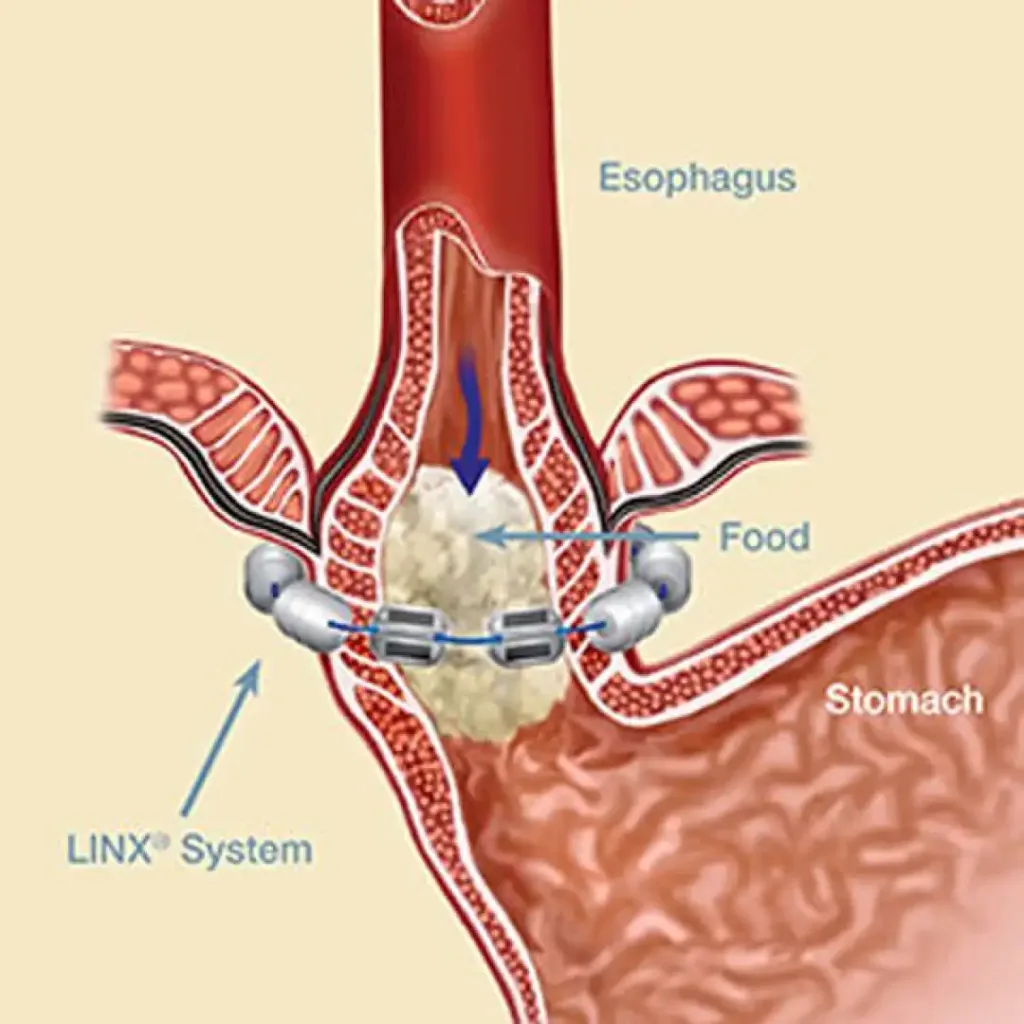
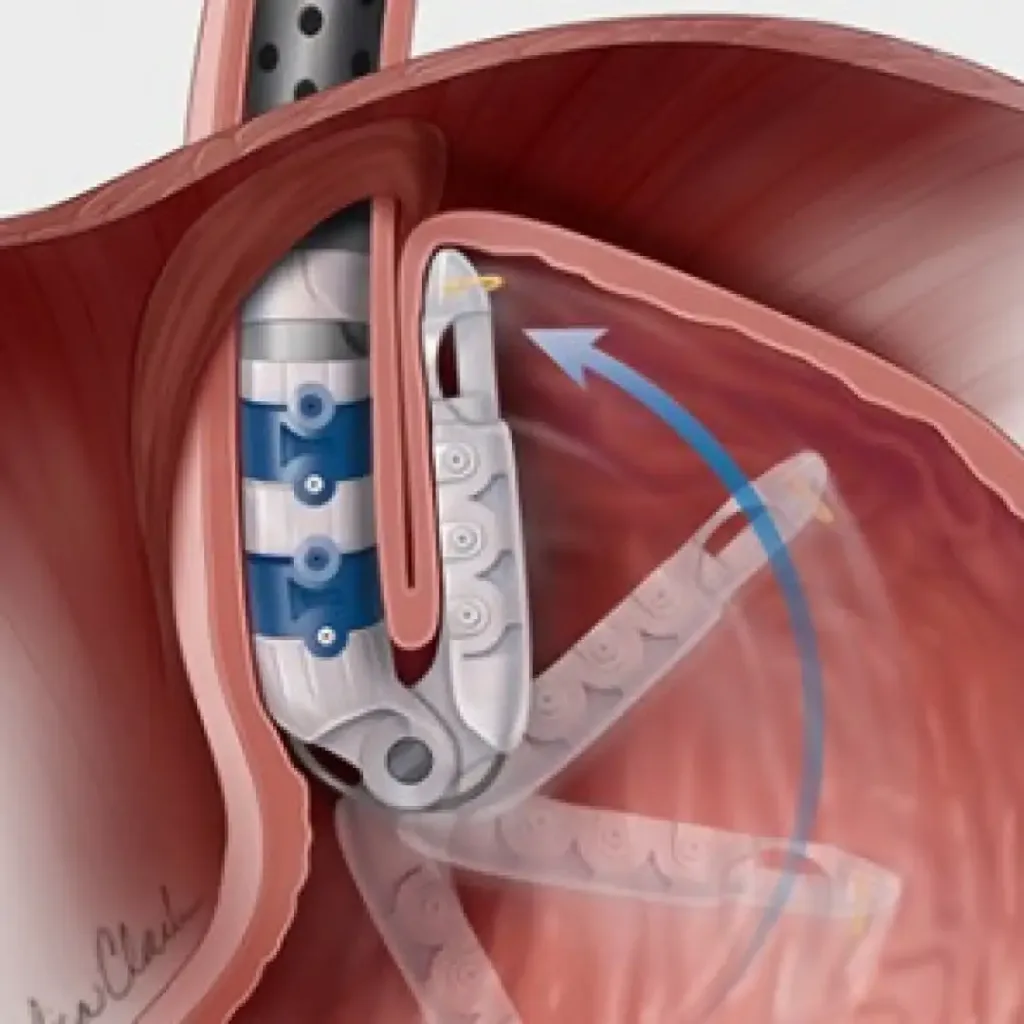
The LINX procedure involves implanting a small, flexible ring of magnetic beads around the lower esophagus. This magnetic ring augments the strength of the LES, preventing the backflow of stomach acid into the esophagus while maintaining normal swallowing capabilities.
Key Features:
- Minimally Invasive: The LINX procedure is minimally invasive, often performed using laparoscopy with small incisions, leading to quicker recovery times.
- Magnetic Beads: The magnetic beads aid in fortifying the LES without compromising the natural swallowing process, providing an effective barrier against reflux.
Considerations:
- Patient Selection: Ideal for individuals with persistent GERD despite optimal medical management.
- Preoperative Assessment: Evaluation includes imaging studies and esophageal motility studies to ensure suitability for the LINX procedure.
- Potential Benefits: Reduced invasiveness, quick recovery, and effective reflux control are key benefits.
- Postoperative Care: Emphasizes returning to normal dietary habits with the newfound protection against reflux.
Schedule an appointment
LINX Procedure: Minimally Invasive Relief for Reflux Read More »