COVID and Acid reflux
Gastroenterology
COVID and Acid reflux
The COVID-19 pandemic has not only affected millions of lives but also brought to light many complications and long-term health effects associated with the virus. One such intriguing connection has emerged between COVID-19 and acid reflux disease. Acid reflux, characterized by the backward flow of stomach acid into the oesophagus, often leads to symptoms like heartburn, regurgitation, and a persistent cough. Understanding the intricate link between COVID-19, cough, and reflux is essential to comprehending this virus’s complex and evolving nature.
COVID-19 and the Coughing Conundrum
COVID-19, caused by the SARS-CoV-2 virus, is primarily known for its respiratory symptoms. Coughing is a common symptom that can persist even after other symptoms have subsided. This persistent cough can be challenging for individuals in many ways, especially when it contributes to developing or exacerbating acid reflux disease.
The Cough-Reflux Connection
- Viral Infection and Cough: The SARS-CoV-2 virus primarily infects the respiratory tract, leading to inflammation and damage to lung tissues. In response, the body’s natural defence mechanism triggers a cough to clear mucus and irritants. Persistent coughing can be distressing for individuals who experience it during or after a COVID-19 infection.
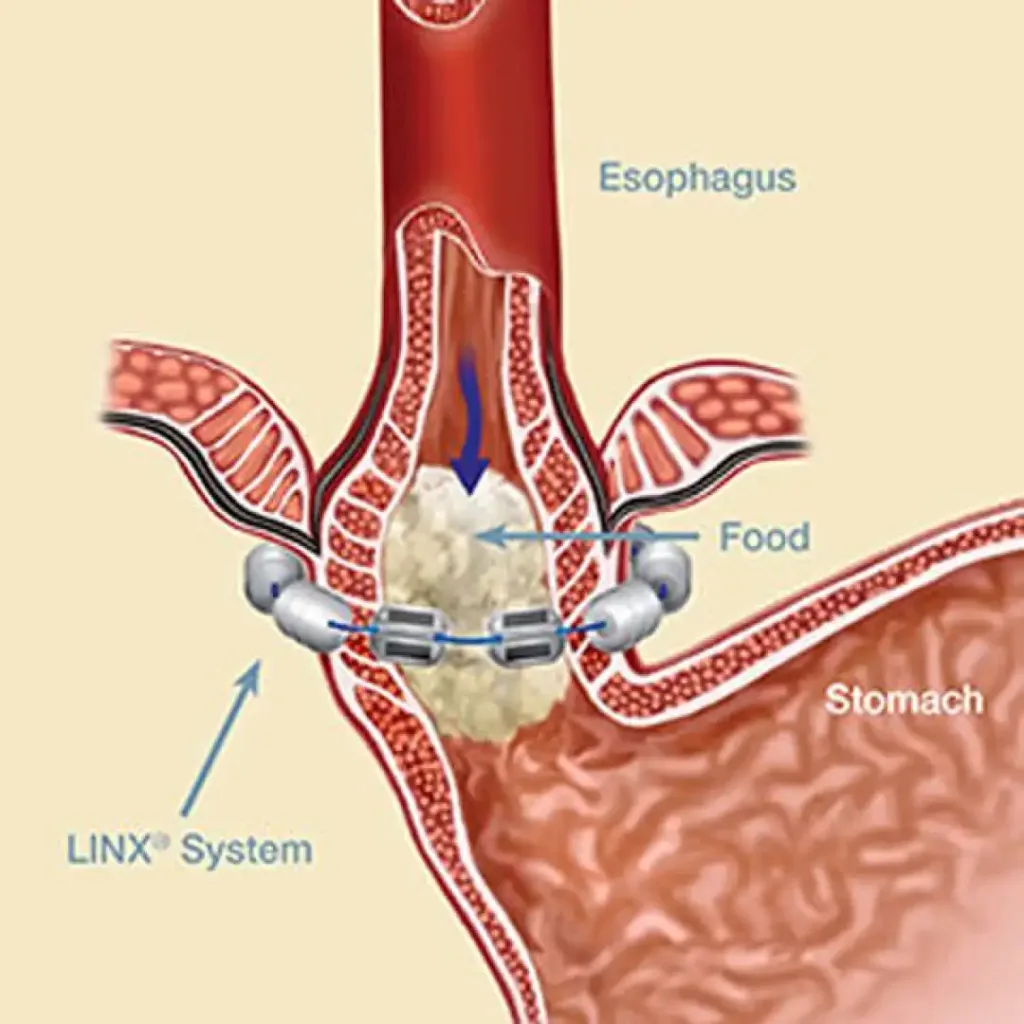
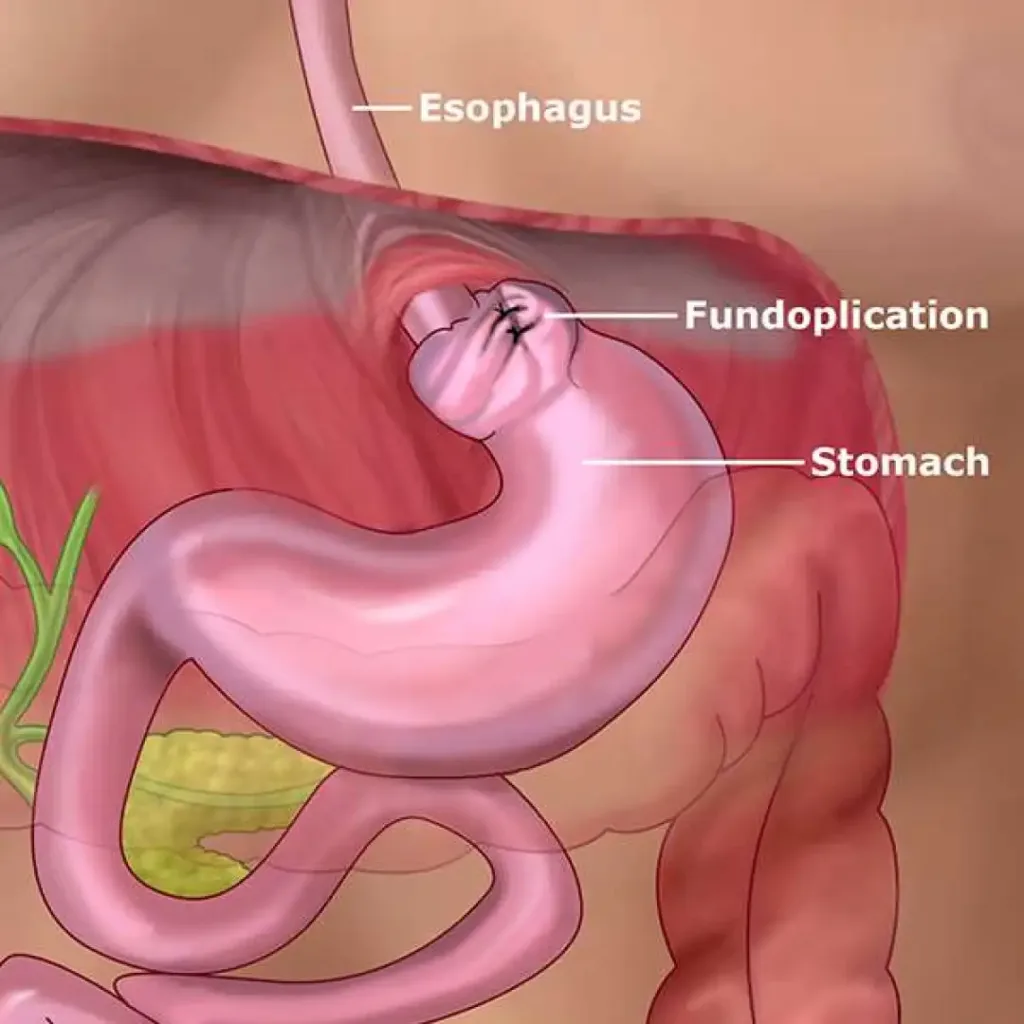
- Increased Intra-abdominal Pressure: Coughing is a forceful action that increases intra-abdominal pressure, causing a surge in pressure within the stomach. This pressure, if consistently high, can force stomach acid to move back up the oesophagus, leading to acid reflux. When the lower oesophagal sphincter, a muscular ring that separates the oesophagus from the stomach, weakens or relaxes inappropriately, it becomes more susceptible to acid reflux events, especially during coughing fits.
- Impact on the Lower Esophageal Sphincter (LES): Frequent coughing may lead to microtrauma in the lower oesophageal sphincter, further weakening its ability to remain tightly closed. When the LES loses its competence, it becomes a less effective barrier against the regurgitation of stomach acid.
- Medications and Their Role: Many individuals suffering from COVID-19 symptoms or related coughing may be prescribed medications like corticosteroids to reduce inflammation. These medications can also weaken the LES and contribute to acid reflux.
Managing Acid Reflux in the Context of COVID-19
Managing acid reflux in the context of COVID-19 requires a multifaceted approach:
- Lifestyle Modifications:
- Maintain a healthy weight to reduce abdominal pressure.
- Elevate the head of the bed to prevent acid from flowing back into the esophagus.
- Avoid large meals, especially before bedtime.
- Limit trigger foods and beverages such as spicy foods, citrus, and caffeine.
- Refrain from smoking and excessive alcohol consumption.
- Medications:
- Proton pump inhibitors (PPIs) or H2-receptor antagonists can help reduce stomach acid production.
- Antacids can provide temporary relief from heartburn symptoms.
- Breathing Techniques:
- Learn to manage and control coughing fits, potentially reducing the strain on the LES.
- Consult a Healthcare Professional:
- If cough and reflux symptoms persist, seek medical advice. A healthcare provider can evaluate your condition and recommend appropriate treatments.
Schedule an appointment
COVID and Acid reflux Read More »