GERD or GORD
Conditions
What is Acid reflux?
Acid reflux, also known as gastroesophageal reflux disease (GERD), is a condition in which stomach acid flows back into the esophagus, causing heartburn and other symptoms. The esophagus is the tube that connects the mouth to the stomach.
In a normal digestive system, a ring of muscle at the bottom of the esophagus called the lower esophageal sphincter (LES) opens to allow food and liquid to flow into the stomach, and then closes to prevent the contents of the stomach from flowing back into the esophagus. However, in people with acid reflux, the LES is weak or relaxed, allowing stomach acid to flow back into the esophagus.
Common symptoms of acid reflux include heartburn, regurgitation, chest pain, and difficulty swallowing. If left untreated, acid reflux can cause damage to the esophagus and increase the risk of developing other health problems, such as esophageal cancer.
Treatment for acid reflux may include lifestyle changes, such as avoiding trigger foods and losing weight, as well as medications to reduce acid production and heal the esophagus. In severe cases, surgery may be recommended to tighten the LES and prevent acid reflux.
If you are experiencing symptoms of acid reflux, it is important to consult with a healthcare provider for an accurate diagnosis and appropriate treatment plan.
How can I cure acid reflux without medications ?
There are several lifestyle changes that can help to reduce the symptoms of acid reflux and avoid the need for medication:
- Lose weight: Extra weight puts pressure on the stomach and can cause acid to leak back into the esophagus.
- Avoid trigger foods: Common trigger foods include citrus, tomato-based products, chocolate, alcohol, caffeine, fatty and fried foods, and spicy foods.
- Eat smaller, more frequent meals: Eating smaller, more frequent meals instead of three large meals can help to reduce the amount of pressure in the stomach and reduce the risk of acid reflux.
- Avoid eating close to bedtime: Eating a large meal close to bedtime can cause acid to flow back into the esophagus while lying down.
- Avoid tight-fitting clothing: Wearing tight-fitting clothing can put pressure on the stomach and increase the risk of acid reflux.
- Raise the head of your bed: Elevating the head of your bed can help to prevent acid from flowing back into the esophagus while you sleep.
- Practice relaxation techniques: Stress and anxiety can increase the risk of acid reflux, so practicing relaxation techniques such as deep breathing, meditation, and yoga can be helpful.
- Chew gum: Chewing gum can help to increase saliva production and neutralize stomach acid.
- Drink herbal tea: Drinking herbal tea, such as chamomile or fennel, can help to soothe the digestive system and reduce symptoms of acid reflux.
It’s important to note that these lifestyle changes may not work for everyone, and some people may still require medication to manage their symptoms. It’s always best to consult with a healthcare provider to determine the best treatment plan for you.
How to diagnose acid reflux?
Acid reflux can be diagnosed through a combination of medical history, physical examination, and diagnostic tests. Some common tests used to diagnose acid reflux include:
- Esophagogastroduodenoscopy (EGD): This test involves inserting a flexible scope with a camera through the mouth into the esophagus, stomach, and small intestine to visualize any damage or irritation caused by acid reflux.
- pH monitoring: This test involves placing a device in the esophagus to measure the acidity of the esophagus and track when symptoms occur.
- Barium swallow X-ray: This test involves drinking a chalky liquid that helps to highlight any abnormalities in the esophagus and stomach, such as narrowing or blockages caused by acid reflux.
- Chest X-ray: A chest X-ray can help rule out other possible causes of chest pain or discomfort, such as a lung problem.
- Blood tests: Blood tests may be done to check for anemia, which can be a sign of acid reflux-related damage to the esophagus.
Your doctor may also ask about your symptoms and medical history, including what you eat, how often you experience symptoms, and if you take any medications. This information can help your doctor determine if you have acid reflux and what treatment options may be best for you.
Surgical options for acid reflux
There are several surgical options available for treating acid reflux and gastroesophageal reflux disease (GERD). The surgical options include:
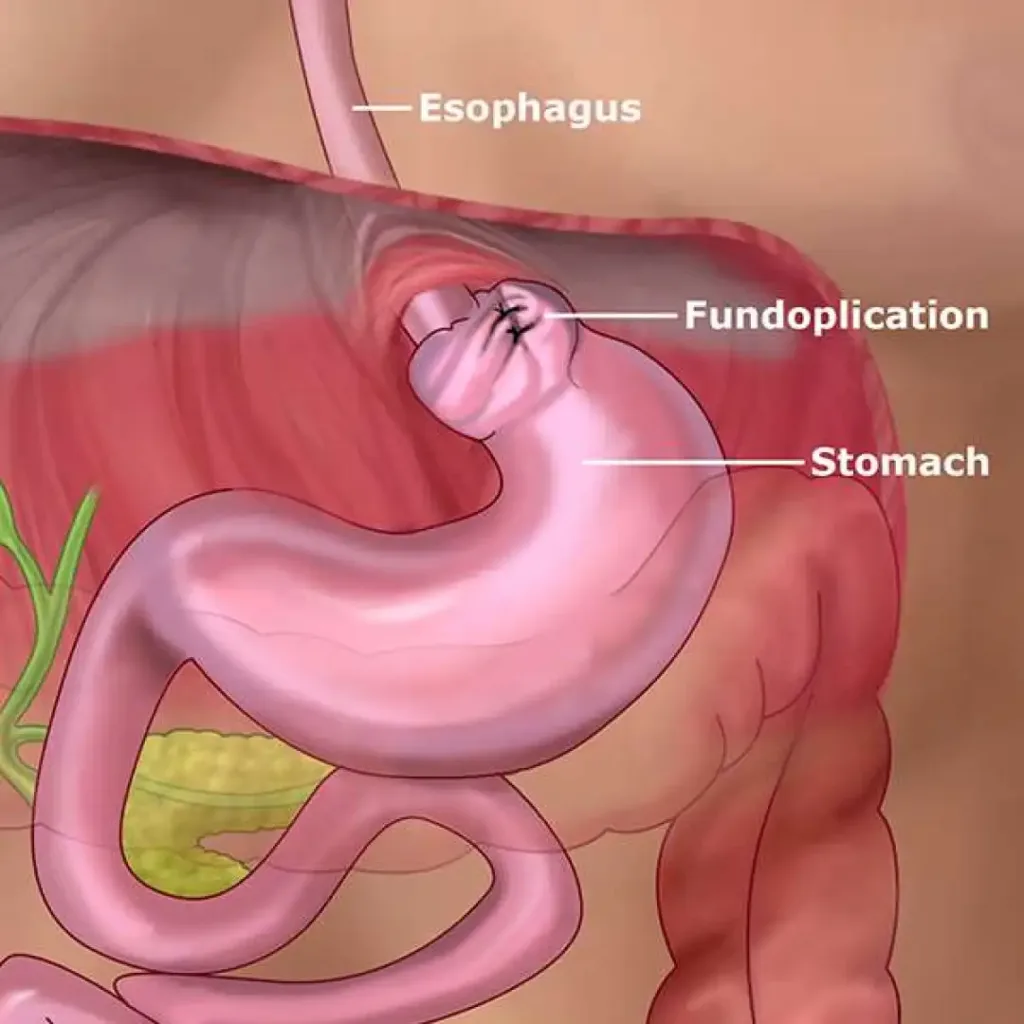
- Fundoplication: This is the most common surgical procedure for treating GERD. It involves wrapping the top part of the stomach around the lower esophagus to create a barrier that prevents acid from flowing back into the esophagus.
- Transoral Incisionless Fundoplication (TIF): This is a minimally invasive procedure that uses an endoscope (a thin, flexible tube with a camera) to create a tight valve at the base of the esophagus. TIF is performed through the mouth and does not require any incisions.
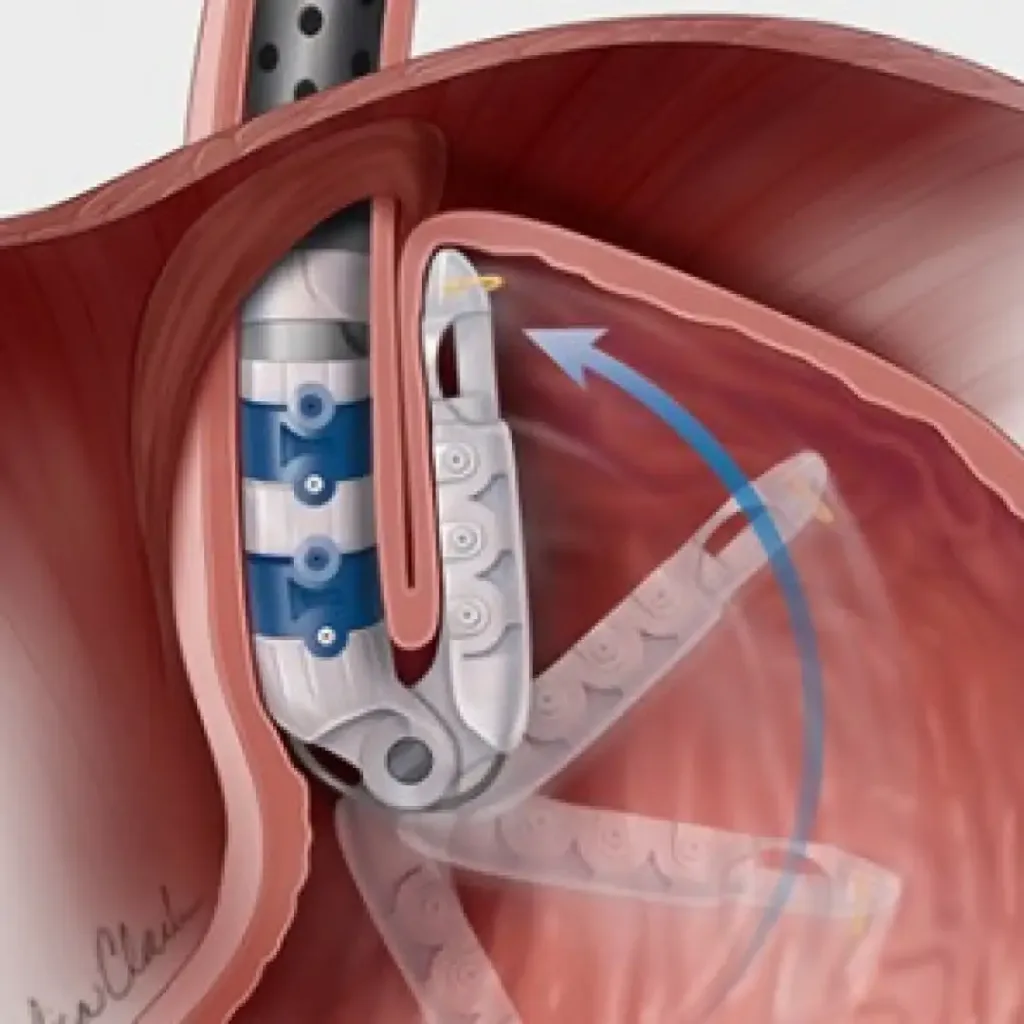
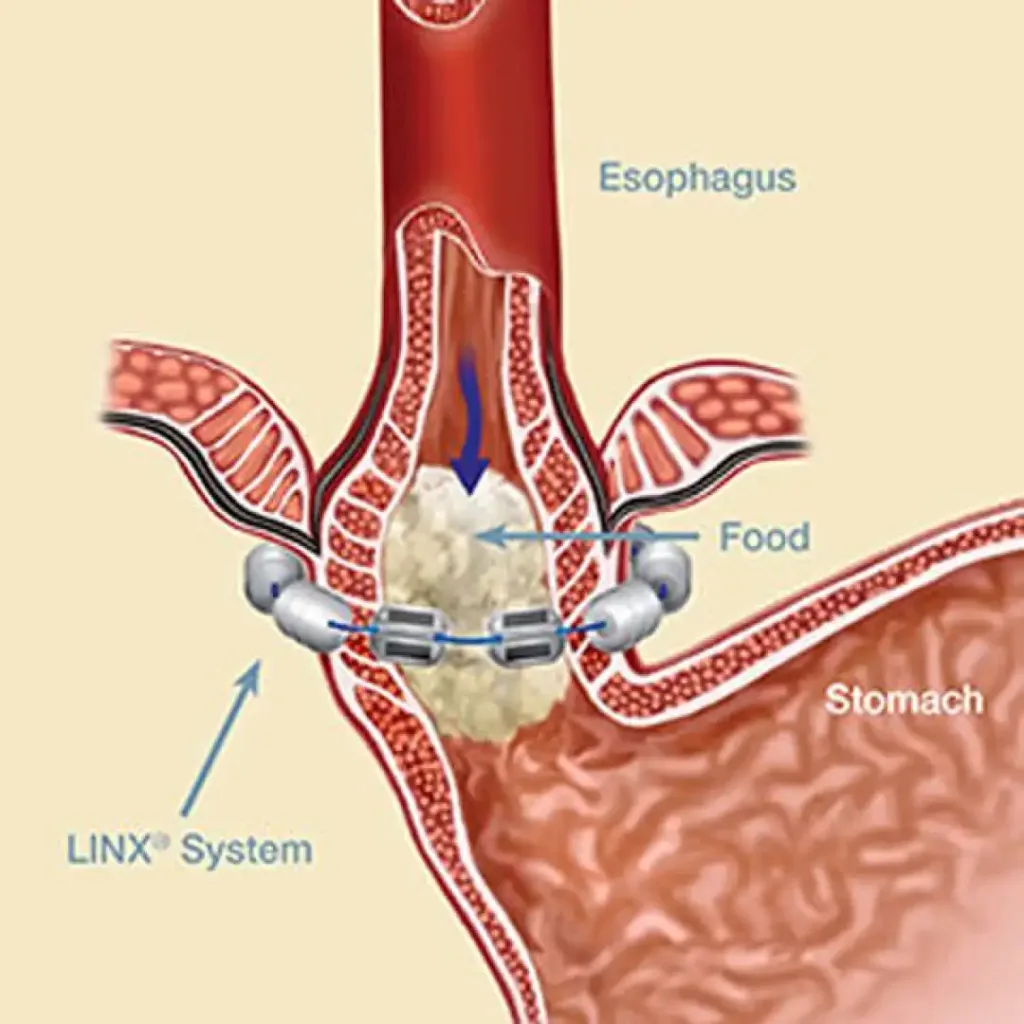
- LINX® Reflux Management System: This is a small device made of magnetic beads that is placed around the lower esophageal sphincter (LES) to help prevent acid from flowing back into the esophagus.
- Nissen Fundoplication: This is a more extensive form of fundoplication that involves wrapping the entire circumference of the stomach around the esophagus. Nissen fundoplication is typically used for more severe cases of GERD.
- Gastric inlet patch: This procedure is used to treat a specific type of hernia called a hiatal hernia, which can contribute to acid reflux. The procedure involves placing a patch or mesh over the hernia to reinforce the weakened area of the diaphragm and prevent the hernia from recurring.
Surgical options for acid reflux are typically recommended for patients who have not responded to other treatments, such as lifestyle changes and medications, or for patients with severe or complicated cases of GERD. The success rate of these procedures is high, and most patients experience significant relief from their symptoms after the surgery. However, as with any surgical procedure, there are potential risks and complications that should be discussed with your doctor prior to the surgery.
What is Bravo acid reflux testing?
Bravo pH testing is a type of diagnostic test used to measure the acidity in the esophagus over an extended period of time. It is used to diagnose gastroesophageal reflux disease (GERD) and other acid reflux-related conditions.
The Bravo test involves the placement of a small capsule in the esophagus, near the lower esophageal sphincter. The capsule is attached to a thin wire and remains in place for two to three days. During this time, it measures the pH levels in the esophagus and sends the data to a recorder worn on a belt around the waist.
The data from the Bravo test can help determine the frequency, duration, and severity of acid reflux and provide information that can help guide treatment decisions. The test is usually performed when other diagnostic tests, such as a traditional pH monitoring test or an endoscopy, have not provided a clear diagnosis or have not accurately measured the severity of acid reflux symptoms.
What is oesophageal high resolution manometry?
Oesophageal high-resolution manometry (HRM) is a diagnostic test used to evaluate the muscle contractions and pressure changes within the esophagus. It is used to diagnose and evaluate a variety of digestive disorders, particularly those affecting the oesophagus, including gastroesophageal reflux disease (GERD), achalasia, and other motility disorders.
HRM is a specialized form of manometry that provides a more detailed and accurate assessment of the functioning of the esophagus. It uses a specialized catheter that is inserted through the nose or mouth and into the esophagus. The catheter contains multiple sensors that measure the pressure and contractions of the esophageal muscles.
The results of HRM can help diagnose digestive disorders, determine the cause of symptoms, and guide treatment decisions. The test is usually performed when other diagnostic tests, such as an endoscopy or a traditional manometry test, have not provided a clear diagnosis or have not accurately measured the severity of symptoms.
What is Barrett’s oesophagus?
Barrett’s esophagus is a condition in which the normal tissue lining the lower part of the esophagus (the tube that carries food from the mouth to the stomach) is replaced with abnormal tissue. It is a complication of gastroesophageal reflux disease (GERD), a condition in which stomach acid and other contents flow back into the esophagus.
The abnormal tissue in Barrett’s esophagus is believed to be a response to the irritation and damage caused by repeated exposure to stomach acid. In some cases, this abnormal tissue can develop into a type of pre-cancerous condition called dysplasia.
Symptoms of Barrett’s esophagus can include heartburn, difficulty swallowing, and chest pain. The condition is usually diagnosed through endoscopy, a procedure in which a lighted scope is used to examine the esophagus and stomach. Treatment for Barrett’s esophagus typically involves medications to control GERD and prevent further irritation to the esophagus, as well as periodic endoscopic surveillance to monitor for the development of dysplasia. In some cases, treatment may involve removal of the abnormal tissue.
What are the risks of obesity?
Obesity is defined as having a body mass index (BMI) of 30 or higher, and it is associated with several serious health risks, including:
- Cardiovascular disease: Obesity increases the risk of heart disease, stroke, high blood pressure, and high cholesterol.
- Type 2 diabetes: Obesity is a leading risk factor for the development of type 2 diabetes.
- Cancer: Obesity increases the risk of several types of cancer, including breast, colon, endometrial, kidney, and esophageal cancer.
- Sleep apnea: Obesity is a major risk factor for the development of sleep apnea, a serious sleep disorder that can cause fatigue, decreased productivity, and other health problems.
- Joint problems: Obesity can increase the risk of joint problems, such as osteoarthritis, as extra weight puts stress on joints and cartilage.
- Liver disease: Obesity can increase the risk of liver disease, such as nonalcoholic fatty liver disease and cirrhosis.
- Gallbladder disease: Obesity increases the risk of gallstones and other gallbladder problems.
- Mental health problems: Obesity is associated with an increased risk of depression, anxiety, and other mental health problems.
- Reproductive problems: Obesity can cause infertility and increase the risk of complications during pregnancy and childbirth.
It’s important to maintain a healthy weight to reduce the risk of these and other health problems. This can be achieved through a combination of healthy eating, regular physical activity, and a commitment to a healthy lifestyle.
How can I lose weight?
Here are some strategies for losing weight:
- Eat a balanced diet: Focus on eating a balanced diet that includes plenty of fruits and vegetables, lean protein, whole grains, and healthy fats. Limit your intake of sugar, salt, and unhealthy fats.
- Reduce portion sizes: Pay attention to the portion sizes of the foods you eat, and try to reduce the amount of food you consume at each meal.
- Avoid high-calorie drinks: Limit your intake of high-calorie drinks such as soda, fruit juice, and sweetened coffee or tea.
- Increase physical activity: Try to get at least 30 minutes of physical activity most days of the week. This can include walking, cycling, swimming, or any other form of exercise that you enjoy.
- Get enough sleep: Aim for 7-8 hours of sleep per night to help regulate your metabolism and reduce stress levels, which can both contribute to weight gain.
- Practice mindful eating: Pay attention to your hunger and fullness signals and eat slowly and without distractions. This can help you be more mindful of what and how much you are eating.
- Reduce stress: High levels of stress can lead to overeating and weight gain. Try to find healthy ways to manage stress, such as exercise, meditation, or talking to a therapist.
- Get support: Consider joining a weight loss support group or working with a registered dietitian or personal trainer to help you stay on track.
Remember, weight loss is a gradual process and it’s important to be patient and kind to yourself. It’s also important to consult with a healthcare professional before starting any weight loss program, especially if you have any underlying medical conditions.
Why do people do not stick to diet and exercise?
There are many reasons why people may struggle to stick to a diet and exercise plan. Some common reasons include:
- Lack of motivation: People may lose their initial motivation to eat healthier or exercise regularly over time.
- Lack of time: Many people have busy schedules and finding time for exercise or preparing healthy meals can be a challenge.
- Lack of variety: Eating the same foods repeatedly or doing the same exercises over and over can get boring, leading people to abandon their diet or exercise plan.
- Emotional eating: Some people turn to food for comfort or as a way to cope with stress, making it difficult to stick to a healthy diet.
- Unrealistic expectations: Setting unrealistic goals or expectations can lead to disappointment and frustration, which can cause people to abandon their diet or exercise plan.
- Stress: High levels of stress can disrupt eating and exercise habits, making it difficult to stick to a plan.
- Social pressure: Going against the norm, such as ordering a salad instead of a burger at a social gathering, can be difficult and cause people to abandon their healthy habits.
- Travel: Traveling can make it difficult to stick to a diet and exercise plan, as you may be in a new place with limited access to healthy foods or opportunities for physical activity.
It’s important to find ways to overcome these challenges and maintain a healthy lifestyle. For example, finding an accountability partner, tracking progress, and finding healthy ways to manage stress can help you stay on track.
What are the medications for weight loss?
There are several types of medications that can be used for weight loss, including:
- Orlistat (Xenical): This medication works by blocking the absorption of fat in the gut, leading to fewer calories being absorbed and stored as fat.
- Liraglutide (Saxenda): This medication is a glucagon-like peptide-1 (GLP-1) receptor agonist that helps regulate appetite and reduces food cravings.
- Bupropion/naltrexone (Contrave): This medication is a combination of an antidepressant and an opioid antagonist, and it helps regulate appetite and reduce cravings for food.
- Phentermine (Adipex-P, Ionamin): This medication is an appetite suppressant that works by decreasing hunger and increasing feelings of fullness.
- Lorcaserin (Belviq): This medication works by activating certain brain receptors that control appetite and food intake.
It’s important to note that these medications should not be used as a sole method of weight loss, but rather as part of a comprehensive weight loss program that includes a healthy diet and regular exercise. Additionally, the safety and efficacy of these medications can vary, so it’s important to talk to your doctor to determine the best option for you and to understand any potential risks or side effects.
Surgical options for weight loss
There are several surgical options for weight loss, also known as bariatric surgery, that can help people with obesity lose weight. These procedures are typically recommended for individuals who have not been able to achieve significant weight loss through diet and exercise alone and for those who have a BMI of 40 or higher, or a BMI of 35 or higher with significant obesity-related health problems such as type 2 diabetes or sleep apnea. Some common surgical options for weight loss include:
- Roux-en-Y gastric bypass: This procedure involves creating a small pouch at the top of the stomach and connecting it directly to the small intestine, bypassing the rest of the stomach and part of the small intestine. This reduces the amount of food that can be eaten and the number of calories and nutrients absorbed.
- Sleeve gastrectomy: This procedure involves removing about 80% of the stomach, leaving a sleeve-shaped stomach that is about the size of a banana. This smaller stomach restricts food intake and promotes weight loss.
- Adjustable gastric banding: This procedure involves placing an adjustable band around the upper part of the stomach to create a small pouch that restricts food intake and slows the passage of food into the rest of the stomach.
- Biliopancreatic diversion with duodenal switch: This procedure involves removing a large portion of the stomach and rerouting the small intestine to the remaining portion of the stomach, resulting in significant restriction of food intake and malabsorption of calories.
These surgical options can lead to significant weight loss and improvement in related health conditions, but they are not without risks and side effects, and they also require significant lifestyle changes, including changes to diet and physical activity habits. It’s important to discuss the potential benefits and risks of bariatric surgery with your doctor to determine if it is right for you.