It is possible that a gastrointestinal (GI) problem, such as acid reflux, could be the cause of a mouth sore or ulcer. While occasional sores and ulcers are normal, if you continue to experience them, it is advisable to consult a GP or dentist. After evaluating your symptoms, they may suggest seeing a gastroenterologist to investigate whether a GI condition is contributing to your problems. Our gastroenterologist is available to determine if an upper GI problem is causing your mouth sore or ulcer.
Related Symptoms
- Acid reflux, heartburn, and indigestion
- Cough and throat clearing
- Hoarseness of voice
- Swallowing problems (dysphagia)
What are mouth ulcers and sores?
An ulcer is a type of sore that can occur in various parts of the body, including the mouth. Mouth sores, which are painful lesions, can appear on the lips, gums, tongue, cheeks, and the floor or roof of the mouth.
Mouth sores and ulcers can cause redness, inflammation, and pain, and you may experience just one or many at a time. If you experience multiple ulcers or sores, or they keep returning, it is advisable to consult a healthcare professional.
If you are experiencing severe pain along with a fever, a skin rash, joint pain, or diarrhoea, it is recommended to book an appointment with your doctor. Additionally, seek help if your pain does not improve with medication or you experience no pain.
What do sores and ulcers look like?
A sore or ulcer in the mouth can take on a round or oval shape and may vary in colour depending on the underlying cause. Mouth sores can appear red, white, grey, yellow or purple.
If you notice a white/grey sore with a red halo, it may be a canker sore or aphthous ulcer. These are usually small and oval-shaped and may indicate a folate (vitamin B9) deficiency and anaemia, which are signs of coeliac disease. These sores can be white, grey, yellow or red. Anaemia can cause pale gums and skin.
Patches or lesions in the mouth could be a result of acid reflux, appearing anywhere inside the mouth or on the gums, tongue or palate.
It is important to note that patches or lesions may also be a sign of mouth cancer. These can appear red or white and would not heal. You may also experience persistent lumps in the mouth or neck and unexplained loose teeth. If you experience any of these symptoms, seek medical attention immediately.
Frequent mouth ulcers and sores
Mouth ulcers and sores can have various causes, including minor injuries (trauma), hormonal changes, stress, and underlying medical conditions.
Common causes of mouth sores and ulcers include stress, gum damage, and vitamin deficiencies. Although discomfort may be present for a brief period, healing should occur quickly. If a vitamin deficiency is detected, supplements may be recommended.
If new sores or ulcers continue to appear before the previous ones have fully healed, it is advisable to speak with a healthcare professional. These symptoms may indicate an underlying gastrointestinal condition, particularly an upper GI condition.
Symptoms that indicate an upper GI problem
If your mouth sores or ulcers are due to an upper GI condition, you may experience the following additional symptoms.
- Frequent acid reflux, heartburn, and indigestion
- Abdominal pain and cramping
- Hoarseness of voice
- Constant sore throat
- Difficulty swallowing
- Reduced appetite
- Bloating and gas
Many of these symptoms overlap with various upper GI conditions.
Upper GI conditions linked to mouth sores
- Gastro-oesophageal reflux disease (GORD/GERD)
- Laryngopharyngeal reflux (LPR)
- Barrett’s oesophagus
- Oesophagitis
Other symptoms that indicate a GI condition
Mouth ulcers or sores can be caused by various gastrointestinal conditions, including Crohn’s disease (IBD) and coeliac disease, in addition to upper GI conditions. The following symptoms may be experienced:
- Weight loss
- Chronic diarrhoea
- Frequent constipation
- Feeling sick and vomiting
When to speak to a gastroenterologist
After receiving a visual examination to confirm the presence of mouth sores or ulcers, further investigation may be necessary to determine the underlying cause. Before referring you to a gastroenterologist, your GP or dentist may want to eliminate causes related to your oral hygiene.
If you are experiencing gastrointestinal symptoms, such as the ones mentioned above, you may wish to consult with a gastroenterologist first. Based on your symptoms, our gastroenterologist can recommend the most appropriate tests to diagnose the cause of your sores or ulcers.
Testing
If a patient presents with symptoms of acid reflux in addition to mouth ulcers, a gastroscopy (upper endoscopy) may be performed to investigate the possibility of gastro-oesophageal reflux disease (GORD). To further confirm or rule out GORD, a 96-hour wireless pH capsule (BRAVO) test may also be conducted.
If inflammatory bowel disease (IBD) is suspected, a colonoscopy, as well as blood and stool tests, may be performed. A diagnosis of coeliac disease can be confirmed through blood tests and a biopsy via endoscopy.
Treatment
The treatment for mouth sores and ulcers depends on their type and underlying cause. If mouth ulcers are accompanied by other upper GI symptoms, or if they are recurring, further tests may be necessary to diagnose the root cause of the problem.
For cases where mouth ulcers are the only concern, lifestyle changes such as modifying the diet and reducing stress levels, or over-the-counter medication such as corticosteroid lozenges and anti-inflammatory drugs, may provide relief.
It is not recommended to squeeze the sores, as this can exacerbate pain and lead to scarring.
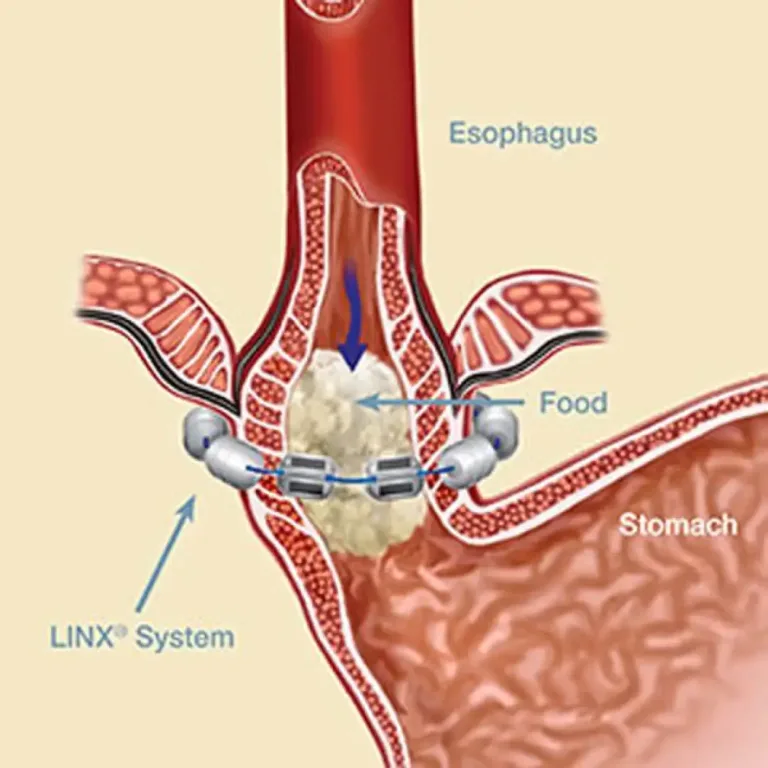
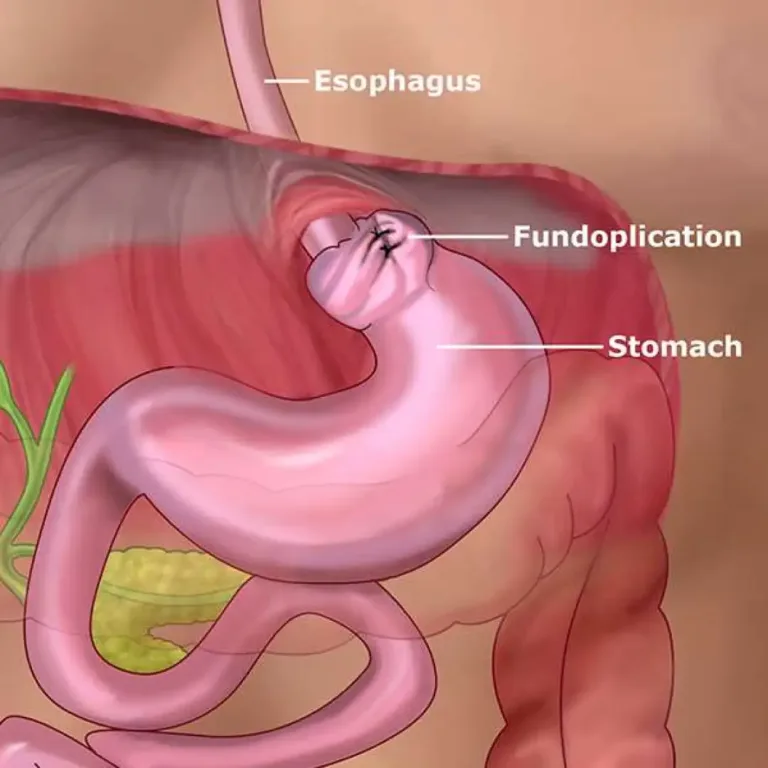
Mouth sores and ulcers are often associated with upper GI conditions that cause acid reflux. In cases where severe acid reflux is the cause of the problem, we may suggest lifestyle changes and medications to reduce reflux. If these methods are ineffective, anti-reflux surgery or other procedures may be recommended.