Understanding the Faecal Calprotectin Test
Gastroenterology
Understanding theFaecal calprotectin test
Faecal calprotectin results provide an objective measure of intestinal inflammation that can help differentiate between inflammatory bowel diseases like ulcerative colitis or Crohn’s disease, and non-inflammatory conditions like irritable bowel syndrome.
The test is useful for evaluating the degree of active intestinal inflammation, monitoring treatment response and disease activity over time. High calprotectin suggests inflammation that may warrant endoscopic evaluation.
Schedule an appointment
Related Articles
Gastroenterology
Understanding the Faecal Occult Blood Test
A faecal occult blood test (FOBT) is a simple,...
Gastroenterology
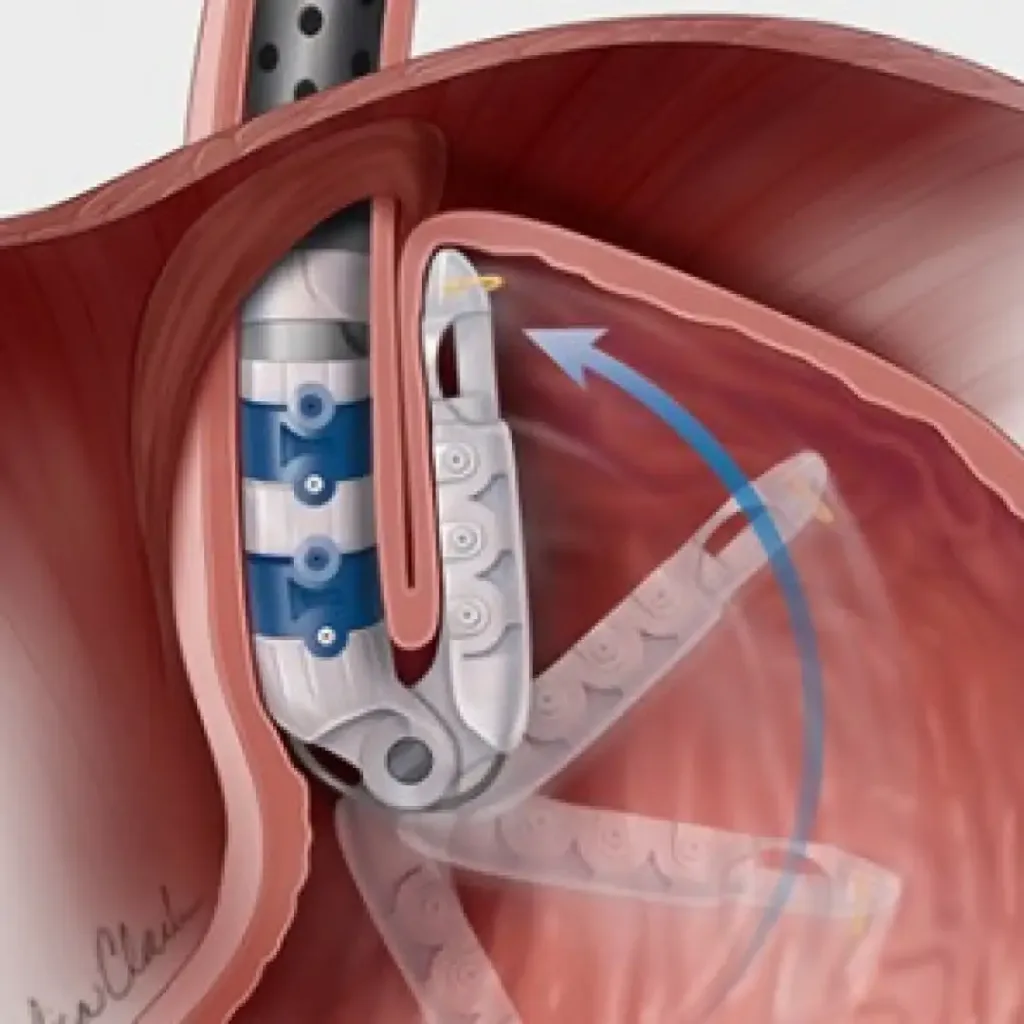
TIF: A New Non-Surgical Option for GERD
For those suffering from chronic acid reflux...
Gastroenterology
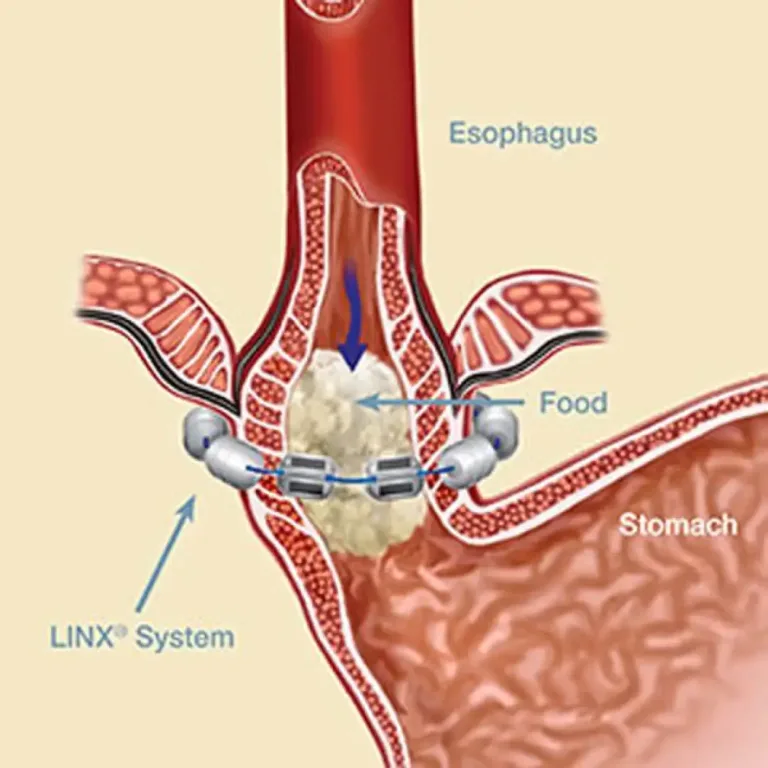
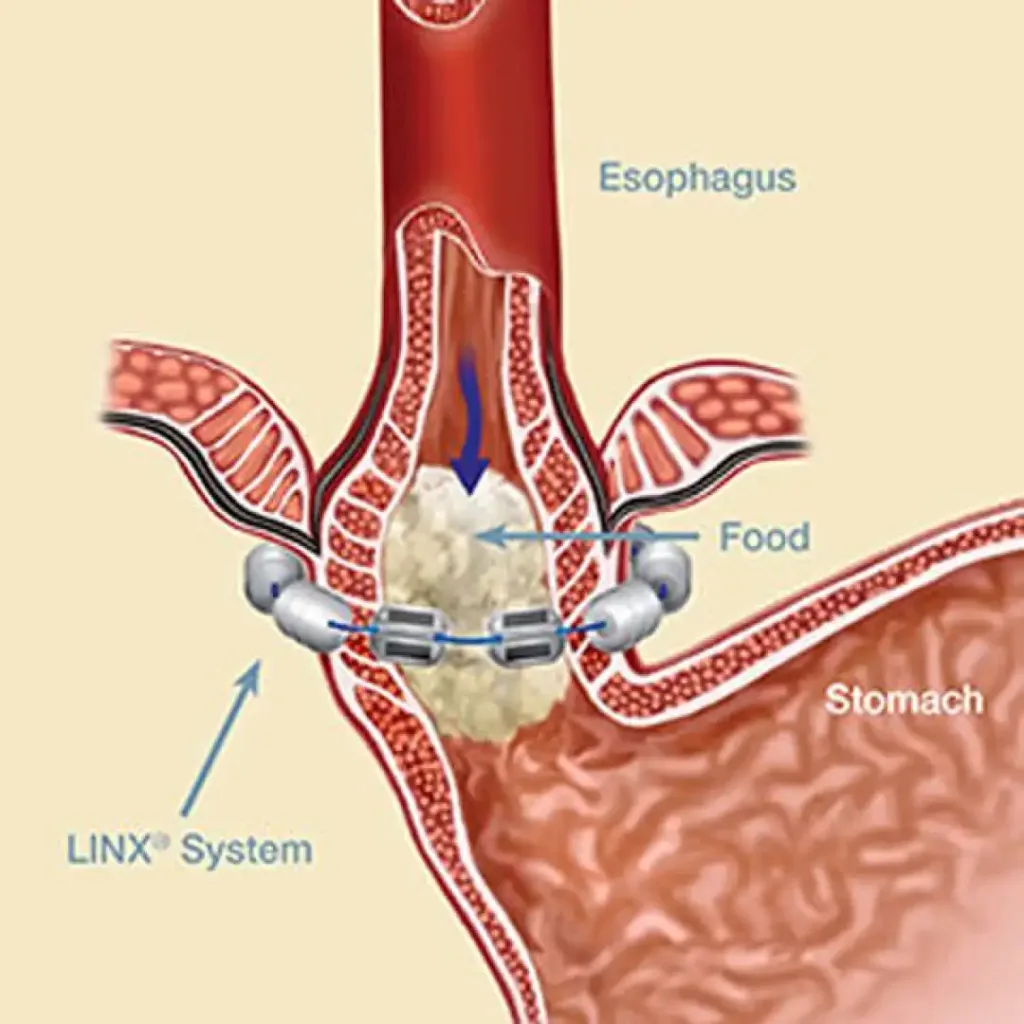
LINX Procedure: Minimally Invasive Relief for Reflux
Offering relief by reinforcing...
Gastroenterology
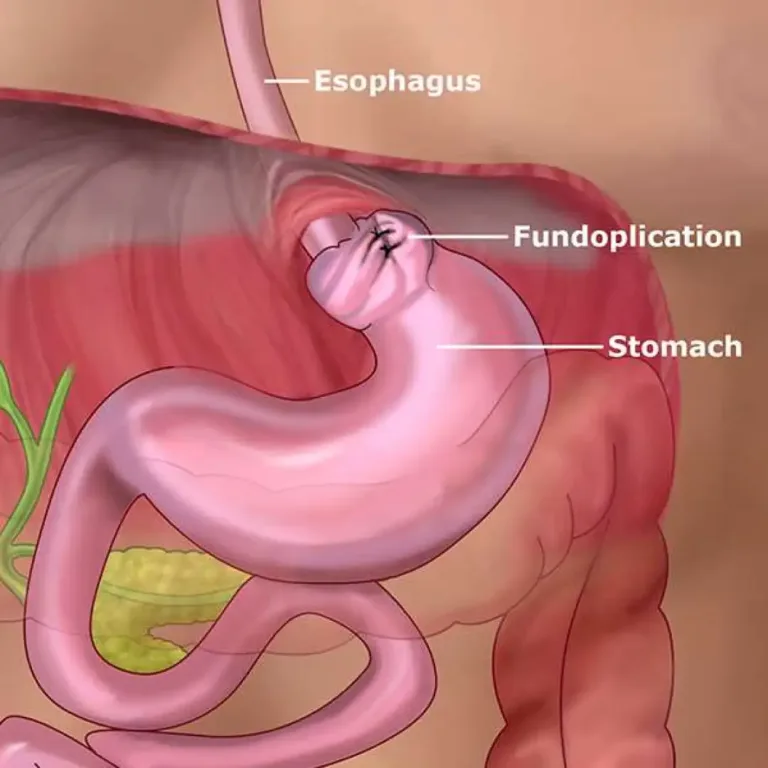
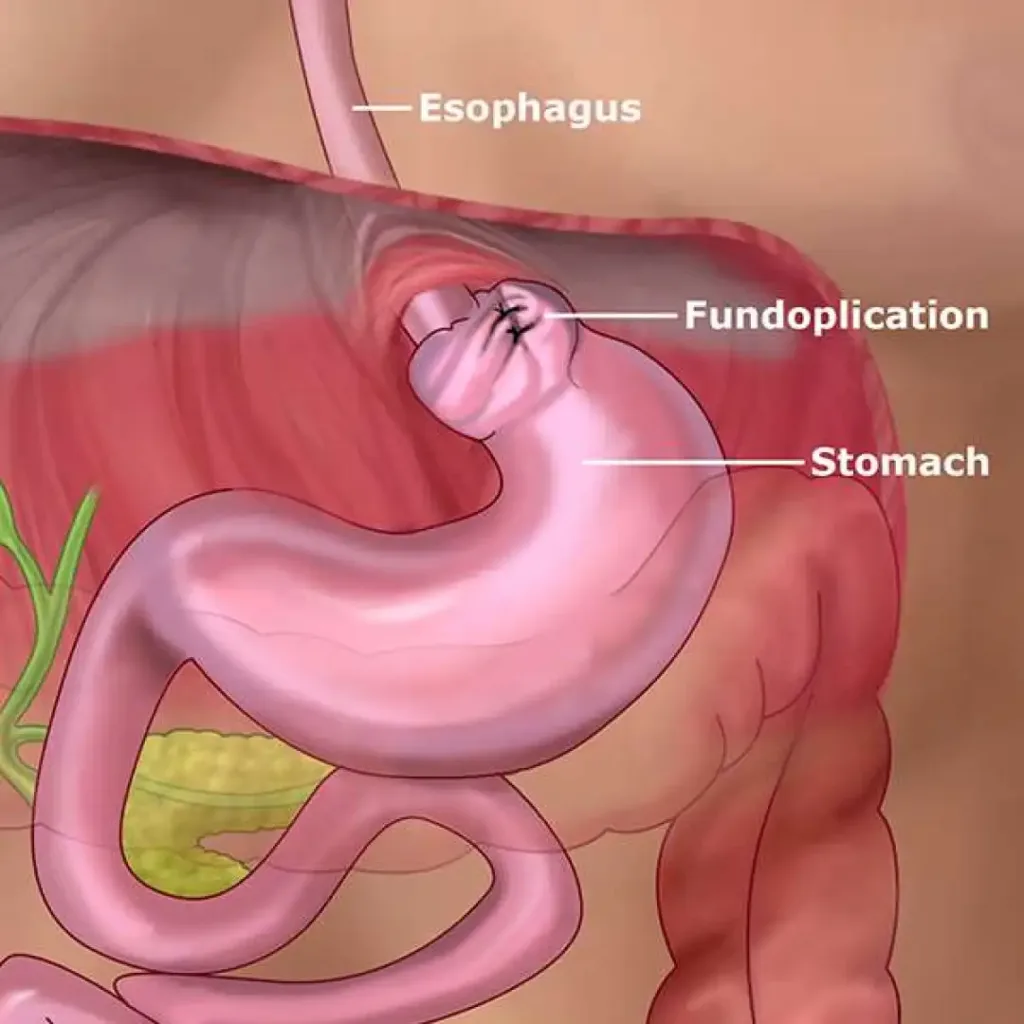
Nissen Fundoplication: A Surgical Solution for Reflux Disease
Nissen fundoplication,...
Gastroenterology
What is Gastroparesis
Gastroparesis, delayed gastric emptying, and issues with stomach...
Gastroenterology
What cannot be seen during an abdominal ultrasound?
While abdominal ultrasound serves...
Understanding the Faecal Calprotectin Test Read More »