Exercising with a temporary gastric balloon
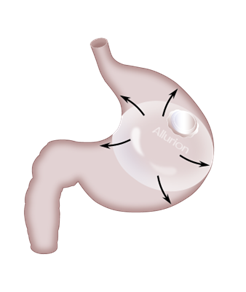
If you are thinking about getting a temporary gastric balloon or if you already have the Allurion Balloon implanted, it is crucial to prioritize an exercise regimen. Engaging in regular physical activity not only promotes mental well-being and physical health, but also aids in managing body weight. While a gastric balloon is a highly effective tool for weight loss as it helps you feel satiated while consuming fewer calories, it is just one component of a comprehensive approach to healthy weight management. Keep reading to discover more about exercising with a weight loss balloon and how the Allurion Programme assists in maintaining motivation.
Can I exercise with a gastric balloon?
Absolutely! Engaging in physical exercise holds significance for everyone as it positively impacts both our mental well-being and physical health. This remains true even if you have undergone a gastric balloon procedure, as it simply facilitates the consumption of smaller meals and enhances your ability to recognize and manage physical hunger.
Moreover, studies indicate that combining dietary modifications with increased physical activity results in a 20% greater weight loss compared to solely altering eating habits.
Maintaining an active lifestyle not only aids in expediting weight loss but, more importantly, it significantly contributes to the sustainability of the lost pounds over the long run. This is primarily due to the fact that exercise plays a crucial role in preserving lean body mass (LBM), which is essential for both short-term and long-term weight management.
In simple terms, LBM can be calculated by subtracting the weight of body fat from the total body weight.
LBM = total body weight – body fat weight
LBM includes muscles, bone mass and bodily fluids etc. Muscles and internal organs use up more calories at rest, than their equivalent weight in fat so a higher LBM percentage helps to boost your metabolism and weight loss efforts.
If you’re on the Allurion Programme or considering getting the Allurion Balloon, the programme includes a range of digital tools to support you in getting fitter or starting a fitness routine.
The Allurion Connected Scale measures body weight, as well as body composition, including fat tissue (% total body weight that consists of fat tissue), visceral fat (fat that is stored around your abdomen) and muscle tissue (% body weight that consists of muscle tissue).
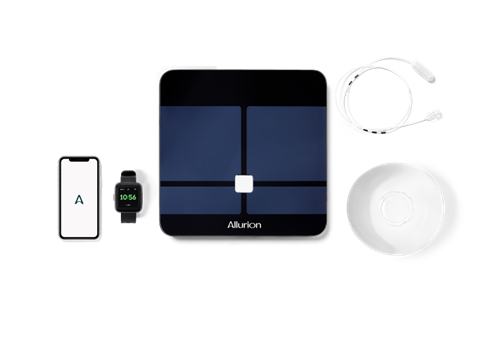
The Allurion Health Tracker enables you to monitor your physical activity and sleep, while the Allurion App allows you to track and monitor your weight, body composition metrics, sleep and fitness activity. Your healthcare team will also have secure access to your data from the app so that they can provide additional support and guidance when needed.
As you’ll see, there are plenty of ways to stay active and healthy while living with a gastric balloon.
When can I start exercising after getting a gastric balloon?
If you’re wondering how soon you can return to your exercise routine after getting a gastric balloon, the answer is sooner than you might think. Placement of the Allurion Balloon is a quick 15-minute procedure which doesn’t require anaesthesia or endoscopy, so you’ll walk away from the clinic pretty much as you went in – plus your 550 ml gastric balloon in situ, of course.
It’s recommended that you avoid strenuous physical activity, like sports, for at least one to two weeks after the balloon has been placed. This will give your body time to adjust to the changes in your intake of fluids and food. As soon as you feel comfortable, you can start leisure walking. During this time, it’s important that you drink enough fluids to ensure you’re adequately hydrated.
Remember that the gastric balloon will reduce the space in your stomach for food and fluids, so it’s important to prioritize taking in enough fluids. You will gradually transition from clear fluids to a normal diet over the course of a week or so with support from your clinic. Keep in mind that everyone is different, so the timeline for these steps may vary.
After your first week post-placement and as you get used to the balloon, you can introduce physical activities (doing things that you enjoy so you’ll be more likely to keep it up) or increase the activities you are already doing (the frequency, intensity and length). Your clinic team can help you set goals that are appropriate for you, and you can use the Allurion Health Tracker to track your progress.
It is important to ensure that you are properly hydrated when you resume your exercise routine, or when you start a new one. During exercise, we lose fluid through sweat and breathing, and if we lose more fluid than we have consumed, it can lead to a negative fluid balance. Signs and symptoms of negative fluid balance include headache, negative mood, and poor concentration. Hence, drinking enough fluids to stay hydrated is a great habit that will support your weight loss and should start as soon as the gastric balloon has been placed.
The key thing to remember regarding exercise, is to start with gentle activities, listen to your body and increase the duration and intensity of what you do when you feel ready. It’s important to take it easy and not push yourself too hard before your body is ready, as this can increase the risk of injury and set you back in your goal to be more active. Your clinic team can work through your goals with you based on your progress and how you feel.
Safe exercises with your temporary gastric balloon
- Walking
- Swimming
- Cycling
- Yoga
- Light circuit training
- Lifting light weights
- Elliptical machine
The benefits of exercise beyond calorie-burning
Exercise benefits overall health. Muscles require ATP for energy. ATP is produced by converting fat stores into energy. Regular exercise helps burn fat and support weight loss. Physical activity improves sleep quality, reduces cravings, and enhances mental health. Exercise increases dopamine and serotonin levels, promoting positive feelings and protecting the brain. The gastric balloon jumpstarts weight loss, but healthier habits are necessary for long-term success. Combining healthy eating and physical activity is more effective for weight loss maintenance. Most people need over 150 minutes of moderate-intensity activity per week. Combining activity with a healthy diet increases success in weight loss. Incorporating exercise and healthy eating is crucial for achieving and maintaining weight loss.
Book a free consultation
Related Articles
Exercising with a temporary gastric balloon Read More »