Non-cardiac chest pain
Conditions
Non-cardiac chest pain
What You Need to Know
Chest pain can be a scary symptom, causing many people to worry that they are having a heart attack. However, chest pain can have a wide range of causes, including non-cardiac issues. In this article, we will explore non-cardiac chest pain, including its causes, symptoms, and treatments.
What is Non-Cardiac Chest Pain?
Non-cardiac chest pain refers to pain in the chest that is not caused by a cardiovascular disorder, such as angina or a heart attack. There are numerous causes of non-cardiac chest pain, including muscular problems, spinal disorders, fractures, lung diseases, anxiety, depression, and digestive issues.
Causes of Non-Cardiac Chest Pain
Muscular problems, such as strained muscles, can cause chest pain that is often described as a sharp, stabbing pain in a specific location. Spinal disorders, such as herniated discs, can also cause chest pain that may radiate to the chest.
Lung diseases, such as bronchitis or pneumonia, can cause pain in the chest that may be accompanied by a cough, shortness of breath, or wheezing. Anxiety, depression, or panic attacks may trigger chest pain that feels like a tightness or pressure in the chest.
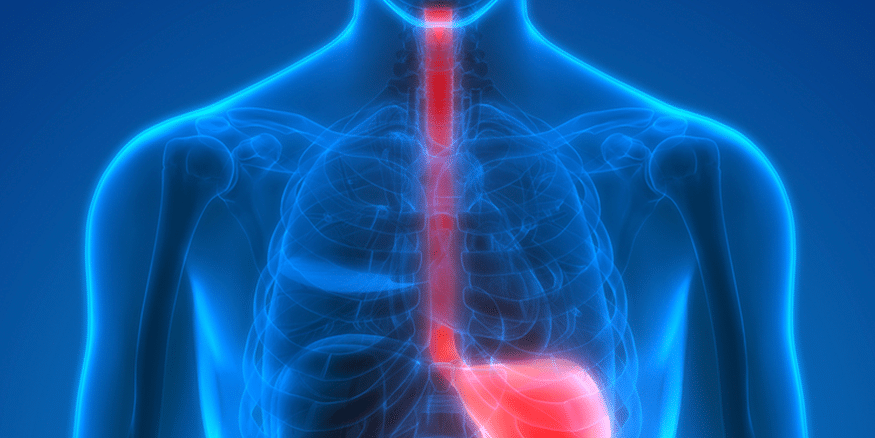
In digestive health, the oesophagus is a possible location of pain in the chest. Gastro-oesophageal reflux disease (GERD) is a common condition that causes acid and bile to rise up the oesophagus from the stomach, causing inflammation and pain. The discomfort will usually feel like burning, which is why it’s described as ‘heartburn’. Other digestive issues, such as stomach ulcers, gallstones, pancreatitis, and inflammatory bowel disease, may also contribute to chest pain.
Symptoms of Non-Cardiac Chest Pain
Symptoms of non-cardiac chest pain can vary depending on the underlying cause. The pain may be specific to one point, a whole side, or more generalised within the chest cavity. The discomfort may feel like burning, stabbing, or pressure. Other symptoms, such as coughing, shortness of breath, nausea, or bloating, may also be present.
Symptoms of Non-Cardiac Chest Pain
Diagnosing non-cardiac chest pain can be challenging, as the symptoms can be similar to those of a heart attack. However, it is important to seek medical attention if you experience sudden chest pain. Your doctor may perform a physical exam, ask about your medical history and symptoms, and order tests, such as gastroscopy, barium swallow, 24-hour pH impedance, high-resolution oesophageal manometry, chest x-ray, or CT scan.
Treating Non-Cardiac Chest Pain
The treatment for non-cardiac chest pain depends on the underlying cause. If the pain is due to muscular problems, rest and pain relief medication may be recommended. Spinal disorders may require physical therapy or surgery. Lung diseases may require medication or oxygen therapy. Anxiety, depression, or panic attacks may be treated with therapy, medication, or relaxation techniques.
In cases where chest pain is caused by GERD, oesophageal muscle relaxants and medications, such as proton pump inhibitors, may be prescribed. In some cases, botox injections may be used to relax the muscles of the oesophagus. Neuromodulators, such as amitriptyline tablets, may be used to treat the pain associated with non-cardiac chest pain.
In conclusion, non-cardiac chest pain can have a wide range of causes, and it is important to seek medical attention if you experience sudden chest pain. Your doctor can perform tests to determine the underlying cause of the pain and recommend appropriate treatment.
Schedule an appointment
Non-cardiac chest pain Read More »