Oesophageal cancer and pre-cancerous lesions
Conditions
Oesophageal cancer and pre-cancerous lesions
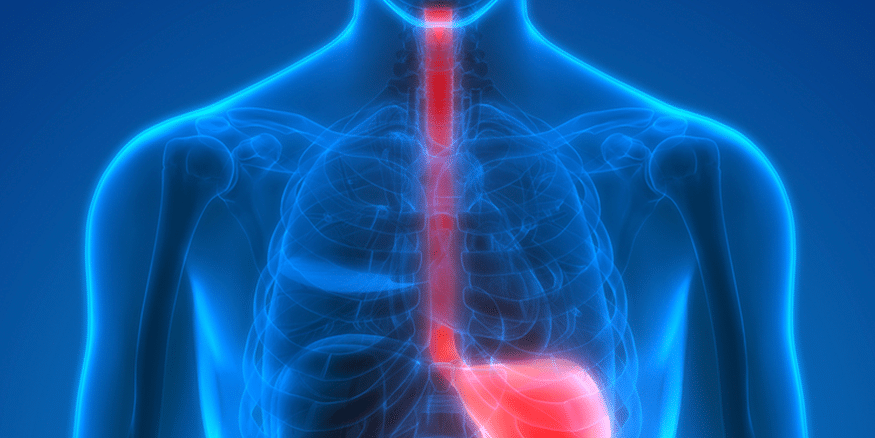
Oesophageal cancer refers to a malignant growth that affects the oesophagus, also referred to as the food pipe or gullet. The symptoms of this condition can be caused by several digestive health conditions, with varying degrees of severity. Although not all symptoms indicate cancer, it is recommended to seek medical attention for any concerning symptoms.
The oesophagus is a tubular organ made of muscles that connects the throat to the stomach, facilitating the passage of food and liquids. Individuals with oesophageal cancer exhibit abnormal cell growth in their oesophagus, which spreads uncontrollably. This type of cancer can develop at any point along the oesophagus.
Symptoms
In the initial stages, oesophageal cancer may not exhibit any noticeable symptoms. However, as the condition progresses, symptoms may start to appear. The cancer usually progresses slowly and forms a tumour that can obstruct the throat as the cells in the oesophagus multiply.
The primary symptoms of oesophageal cancer are:
- Pain in your throat or behind your breastbone
- Bringing food back up (regurgitation)
- Feeling or being sick
- Persistent indigestion or heartburn
- Difficulty swallowing (dysphagia)
- Pain when swallowing
- Feeling or being sick
In the early stages of oesophageal cancer, there may be no noticeable symptoms. However, as the condition progresses, abnormal cell growth in the oesophagus can create a tumour that could potentially obstruct the throat. Some common symptoms of this cancer include experiencing difficulty in swallowing, feeling as if food is stuck in the throat, persistent clearing of the throat, and oesophageal bleeding which can cause coughing up or vomiting of blood, though this is not common. Additionally, stools may appear darker than usual or bloody. Other symptoms may also be present.
Other symptoms include:
- Pain or discomfort in your chest, back or upper abdomen
- Loss of appetite or weight
- A continued cough
- Voice hoarseness
- Tiredness/ fatigue
There are several conditions that can cause the symptoms mentioned above, such as gastro-oesophageal reflux disease (GORD). However, it’s worth noting that having GORD can also raise your risk of developing oesophageal cancer. Therefore, if you experience these symptoms frequently or if your current treatment doesn’t seem to be working, it’s advisable to seek medical attention from your doctor.
Diagnosis
Abnormal cell growth in the oesophagus can result in pre-cancerous lesions, known as dysplasia. During an upper endoscopy, we can extract a sample of this tissue (biopsy) for testing. This test is painless as we numb your throat, and sedation is also an option. To learn more about endoscopy, you can watch this video: “Endoscopy: All You Need to Know”.
If a pathologist identifies signs of high-grade dysplasia, the risk of cancer is higher. Cancer can arise from either of the two main cell types found in the oesophageal lining. As it progresses, cancer may affect the surrounding tissues and organs or spread to other parts of the body. If we detect cancerous cells, we will perform additional tests to determine the stage, grade, and type.
Other tests include a CT scan, PET-CT, endoscopic ultrasound, barium swallow, and laparoscopy. Blood tests may also be necessary. If you experience concerning symptoms, it is important to see your doctor promptly for evaluation.
Types
In medical terms, the type of cell in which cancer originated is known as histology. The two primary histological types of oesophageal cancer are adenocarcinoma and squamous cell carcinoma. Adenocarcinoma is frequently associated with Barrett’s oesophagus and is more common in the UK. In contrast, squamous cell cancer occurs less frequently. Other, less common histological types include small-cell carcinoma, sarcoma, melanoma, lymphoma, and choriocarcinoma. In some cases, we may not be able to identify the specific histological type of cancer, which we refer to as undifferentiated.
Causes
The precise cause of oesophageal cancer remains uncertain. However, it may result from DNA damage in the cells that line the interior of the oesophagus. DNA damage can arise from various lifestyle choices, such as smoking, or prolonged irritation caused by reflux and other medical conditions. Such DNA mutations or alterations may cause cancer. In oesophageal cancer cells, numerous genes may display changes.
Risk factors
The majority of individuals diagnosed with oesophageal cancer are over the age of 60, with men being more frequently affected than women. Other risk factors include being overweight, smoking, or consuming alcohol, particularly more than 14 units per week. Pre-existing conditions such as GORD or Barrett’s oesophagus also increase the risk of developing oesophageal cancer. Additionally, the risk slightly increases after radiotherapy for certain cancers, such as breast, lung, oropharyngeal, or laryngeal cancer. Furthermore, there are reports suggesting that consuming freshly boiled or equally hot drinks may raise the risk of developing oesophageal cancer.
Causes
The precise cause of oesophageal cancer remains unknown. Nevertheless, it is thought to result from DNA damage in the cells that line the interior of the oesophagus. This damage can be caused by certain lifestyle choices, such as smoking, or by chronic irritation from conditions such as reflux. The DNA mutations or changes that result from such damage can lead to the development of cancerous cells. In oesophageal cancer, many genes may undergo changes or mutations.
Treatment
Early stages of oesophageal cancer or pre-cancer can be treated with endoscopic procedures, such as endoscopic resection and HALO radiofrequency ablation, which can remove abnormal tissue and prevent the need for an oesophagectomy (surgical removal of part of the oesophagus). Other treatment options include chemotherapy, radiotherapy, targeted therapy, and immunotherapy.
A multidisciplinary team of highly qualified specialists will work with you to develop a personalised treatment plan based on the stage, grade, and type of cancer.
Schedule an appointment
Oesophageal cancer and pre-cancerous lesions Read More »