What is a private abdominal ultrasound?
Procedures
Ultrasound
What is an abdominal ultrasound?
A private abdominal ultrasound is an ultrasound examination of the abdomen that is performed by a private clinic or hospital, rather than a publicly funded healthcare facility. Patients typically choose a private abdominal ultrasound for a number of reasons, including:
- Quicker access to an appointment: Private healthcare facilities can often provide faster access to an ultrasound appointment compared to the public healthcare system, as there may be shorter waiting lists.
- Increased comfort and privacy: Private clinics and hospitals often offer more comfortable and private facilities compared to the public healthcare system.
- Increased control over the examination: Patients can choose the type of private abdominal ultrasound they would like to have, and they may be able to request a specific radiologist or sonographer.
- More detailed reports: Private clinics and hospitals may offer more detailed reports and results compared to the public healthcare system.
- Increased flexibility: Patients can often choose the time and date of their private abdominal ultrasound appointment, which can be particularly important for those who have busy schedules.
However, it is important to note that private abdominal ultrasounds are typically not covered by healthcare insurance and must be paid for out-of-pocket by the patient. Additionally, private abdominal ultrasounds may not always be necessary, and a referral from a GP or specialist may be required.
What can you see during an abdominal ultrasound?
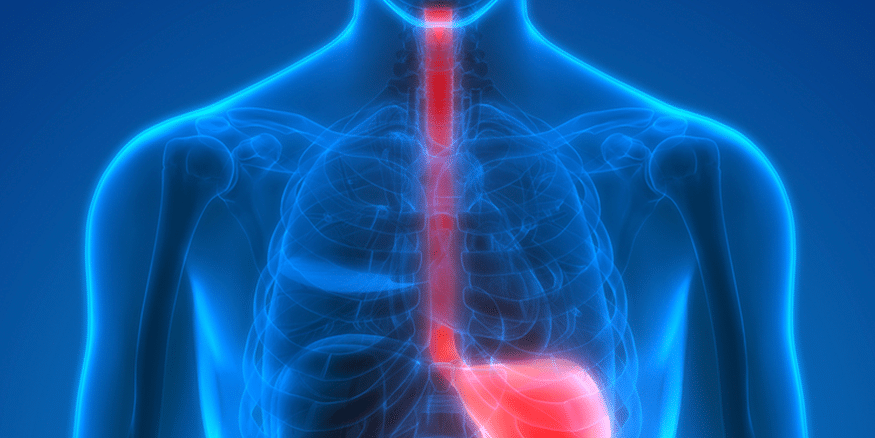
An abdominal ultrasound is a medical imaging test that uses high-frequency sound waves to create images of the organs and tissues within the abdomen. During an abdominal ultrasound, a doctor or a sonographer (technitian) applies a special gel to the patient’s skin and uses a handheld probe to generate the sound waves and capture the images.
An abdominal ultrasound can provide valuable information about the following organs and structures:
- Liver: The ultrasound can assess the size, shape, and texture of the liver and detect any abnormalities, such as cysts, tumors, or cirrhosis.
- Gallbladder: The ultrasound can detect gallstones, evaluate the function of the gallbladder, and identify any inflammation or infection.
- Pancreas: The ultrasound can evaluate the size and shape of the pancreas and detect any abnormalities, such as cysts or tumors.
- Spleen: The ultrasound can assess the size and texture of the spleen and detect any abnormalities, such as an enlarged spleen or a mass.
- Kidneys: The ultrasound can evaluate the size, shape, and texture of the kidneys and detect any abnormalities, such as cysts, tumors, or kidney stones.
- Abdominal blood vessels: The ultrasound can evaluate the blood flow in the major arteries and veins within the abdomen, such as the aorta and the vena cava.
- Abdominal fluid collections: The ultrasound can detect the presence of fluid within the abdomen, such as ascites, which can be a sign of liver disease or other underlying conditions.
In addition to these organs, an abdominal ultrasound can also help diagnose other conditions such as hernias, abdominal pain, and digestive tract problems. The images obtained during an abdominal ultrasound can help guide further diagnostic tests or treatments as needed.
What is a pelvic ultrasound ?
A pelvic ultrasound is a non-invasive diagnostic imaging test that uses high-frequency sound waves to produce images of the structures and organs within the pelvic area, such as the uterus, ovaries, bladder, and prostate gland.
In gastroenterology, a pelvic ultrasound may be used to evaluate the lower gastrointestinal tract, including the rectum and anus, and to assess the structures adjacent to it, such as the bladder and prostate in males, and the uterus and ovaries in females.
Some of the common uses of pelvic ultrasound in gastroenterology include:
Evaluating the extent of rectal cancer: Pelvic ultrasound can help determine the size and location of rectal tumors, and can also identify any nearby lymph nodes that may be affected.
Diagnosing pelvic floor disorders: Pelvic ultrasound can help diagnose pelvic floor disorders, such as fecal incontinence or rectal prolapse, by assessing the anatomy and function of the pelvic muscles.
Assessing prostate enlargement: In males, pelvic ultrasound can be used to assess the size of the prostate gland and to identify any abnormalities, such as enlargement due to benign prostatic hyperplasia or the presence of tumors.
Evaluating urinary incontinence: Pelvic ultrasound can be used to evaluate the bladder and urinary tract to determine the cause of urinary incontinence.
Overall, pelvic ultrasound is a useful diagnostic tool in gastroenterology, as it provides detailed images of the pelvic organs and structures, allowing physicians to accurately diagnose and treat a wide range of gastrointestinal conditions.
Schedule an appointment
What is a private abdominal ultrasound? Read More »