Endometriosis is a persistent medical condition characterised by the growth of cells that bear resemblance to those normally found in the lining of the uterus, in other parts of the body. This chronic disease is known to affect approximately one in ten women and girls of reproductive age and can result in significant debilitation.
Individuals diagnosed with endometriosis typically experience abnormal cellular growth, which reacts in a similar manner to cells found within the uterus, in response to hormonal cycles. Nevertheless, given that these cells are located outside the uterus, the resulting bleeding cannot be expelled from the body as menstrual blood would. This, in turn, causes inflammation, pain, and the formation of scar tissue.
The symptoms of endometriosis can encompass notably painful or heavy menstrual periods, along with feelings of fatigue, depression, and issues relating to bowel, bladder, or fertility.
As it pertains to the digestive system, endometriosis can affect the bowel in two ways: by occurring on the surface of the bowel (referred to as ‘superficial’ endometriosis) or by endometrial cells penetrating the bowel wall (known as ‘deep’ endometriosis).
Bowel endometriosis can produce symptoms akin to those of irritable bowel syndrome, though they typically worsen in the lead up to and during the menstrual cycle, presenting a noticeable pattern. Symptoms may include pain during bowel movements, pain felt deeply in the pelvic region during or after intercourse, and on occasion, rectal bleeding during menstruation.
A range of techniques are employed by clinicians to diagnose endometriosis, such as a vaginal examination, ultrasound scans, or (if deep endometriosis is suspected) CT and MRI scans or surgical intervention to inspect the abdomen or bowel.
Several of the complications resulting from endometriosis can be regulated by painkillers and hormone treatments, which aid in making the associated symptoms more controllable.
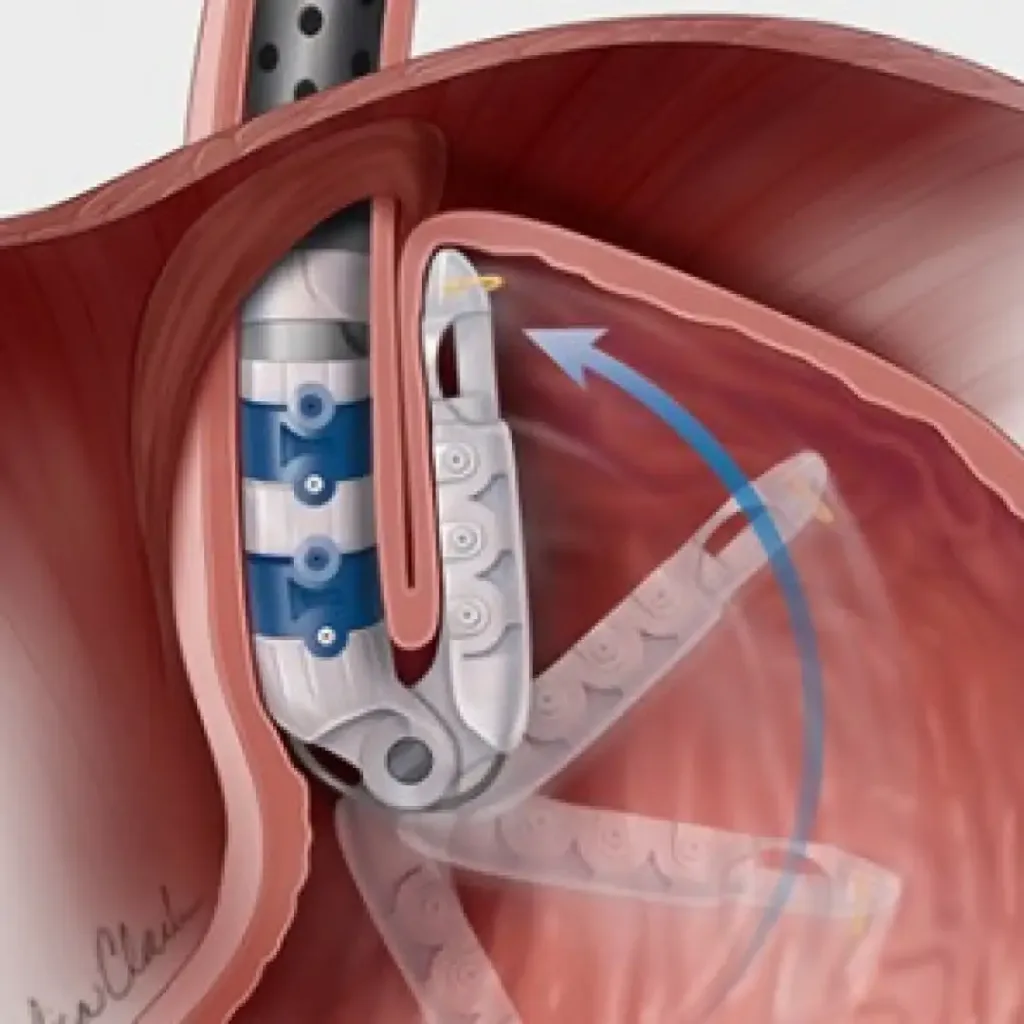
Concerning bowel endometriosis, surgery is typically recommended. The surgical approach taken, whether laparoscopy or open surgery, will depend on the severity of the patient’s condition and the areas affected. Multiple operations may be necessary.
Surgical interventions for this chronic condition are patient-specific and include the option of excising the nodules or affected regions of the bowel, leaving the bowel intact but possibly leaving some endometriosis tissue in place. In cases involving smaller regions of endometriosis, a disc-shaped section of the affected tissue is removed and subsequently sealed. For more severe cases, an affected section of the bowel is excised and then rejoined (a procedure referred to as re-anastomosis).