Belching and burping
Symptoms
Belching and burping
Belching and burping arise due to the presence of excessive air within the oesophagus that is expelled through the mouth. The underlying cause is commonly linked to dietary intake or rapid ingestion. However, persistent occurrences may signify an underlying issue in the upper digestive tract, such as acid reflux. We recommend scheduling an appointment with one of our medical professionals for a thorough examination and diagnosis.
Related Symptoms
What’s the difference between burping and belching?
- - Acid reflux (heartburn) and indigestion
- - Chest pain and discomfort
- - Abdominal pain
- - Bloating
Belching and burping are synonymous in meaning, referring to the act of expelling gas from the mouth, with some regarding belching as producing a more audible sound. An alternative term for this process is eructation.
While typically a natural bodily function, it is only a cause for concern when coupled with other symptoms. If excessive belching and burping persist, we recommend seeking guidance from a medical professional.
As well as trouble swallowing, signs of dysphagia include:
When to seek emergency help
Burping and belching rarely require emergency care, though seek urgent treatment if you experience the following symptoms.
- - Tarry or black stools
- - Severe abdominal pain
- - Sudden difficulty swallowing
- - Blood in your poo (stools) or vomit
- - Vomit that resembles coffee grounds
The manifestation of abrupt swallowing difficulties may indicate an allergic response. Additionally, the presence of blood in vomit or stool may signify internal bleeding within the digestive system.
Causes of burping and belching
Transient episodes of excessive belching may be triggered by the ingestion of specific foods and beverages, including carbonated beverages, curry, chewing gum, and dairy products. Furthermore, temporary burping may also accompany gastrointestinal distress. Nevertheless, persistent belching and burping warrant further evaluation as they could signify an underlying gastrointestinal (GI) ailment requiring medical attention.
Conditions linked to belching and burping
Outlined below are several medical conditions that may give rise to belching and burping, alongside their typical symptoms.
- - Peptic ulcers – also cause blood in your poo
- - Gastritis – can also cause nausea and vomiting
- - Functional or non-ulcer dyspepsia – also causes indigestion
- - H. Pylori – also causes abdominal pain and bloating
- - Gastroparesis – can also cause unintended weight loss
- - Aerophagia – you may experience air gulping and flatulence
- - Food intolerance – symptoms may occur after specific foods
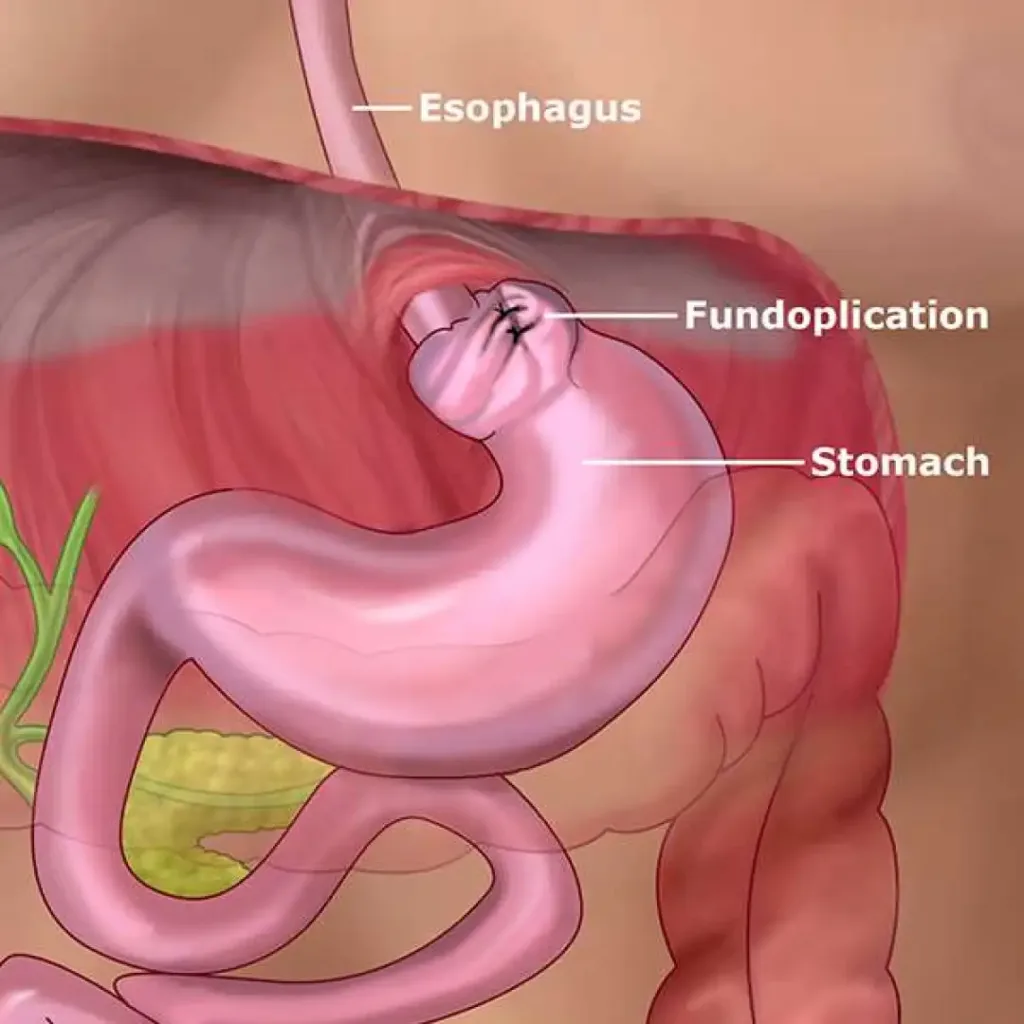
- - Hiatal hernia – may cause bad breath, heartburn and acid reflux
- - Gastro-oesophageal reflux disease (GORD) – frequent acid reflux
- - Irritable bowel syndrome (IBS) – also causes diarrhoea and constipation
Should you present with any of the aforementioned symptoms, we advise seeking guidance from our specialist team to obtain a comprehensive diagnosis.
Diagnosis
The diagnostic approach to identifying the underlying cause of your belching and burping hinges upon the presence of accompanying symptoms. During your consultation, our medical professionals will conduct a thorough evaluation of any additional symptoms, their duration, and possible triggers.
Furthermore, we will delve into your medical history, both personal and familial, to help establish a probable cause for your symptoms. For enhanced visualisation of your digestive system, our specialist may conduct various gastrointestinal (GI) tests.
Testing may involve
- - H. pylori test
- - Maldigestion tests
- - A blood or stool test
- - Hydrogen and methane breath tests
- - Gastroscopy (if we suspect it is GORD)
- - Abdominal scans, such as MRI, CT, or ultrasound scans
Treatment
Prior to seeking professional guidance, there are several lifestyle modifications that you may consider implementing to alleviate belching. Digestive disruptions, including belching, can arise due to poor gut health and heightened stress levels.
If your symptoms cause discomfort, we suggest consulting with a specialist at the earliest convenience. Maintaining a symptom tracker and food diary may prove beneficial in providing our team with an accurate depiction of your condition during your appointment.
After identifying the underlying cause of your symptoms, our specialists will recommend the most suitable course of treatment. In the event that we diagnose a gastrointestinal (GI) ailment, follow-up testing, medication, or surgery may be necessary.
Lifestyle changes to prevent belching and burping
- - Quit smoking
- - Don’t drink through a straw
- - Avoid eating or drinking quickly
- - Eat less fatty or high-fibre foods
- - Try taking a short walk after eating
- - Stop chewing gum or similar products
- - Limit carbonated drinks, such as beer
- - Avoid certain other foods, such as mushrooms, beans, cabbage, broccoli, lentils, onions, and some fruits.
Over-the-counter medications
Some over-the-counter medications may alleviate your symptoms, such as antacids. Your local pharmacist can advise you on the medicines that may help.
Schedule an appointment
Belching and burping Read More »