Gastroenterology
FAQ
Gastroenterology
Q: What is a gastroenterologist?
A: A gastroenterologist is a medical specialist who is trained in the diagnosis and treatment of diseases and conditions that affect the digestive system, which includes the oesophagus, stomach, small intestine, colon, pancreas, liver, and gallbladder.
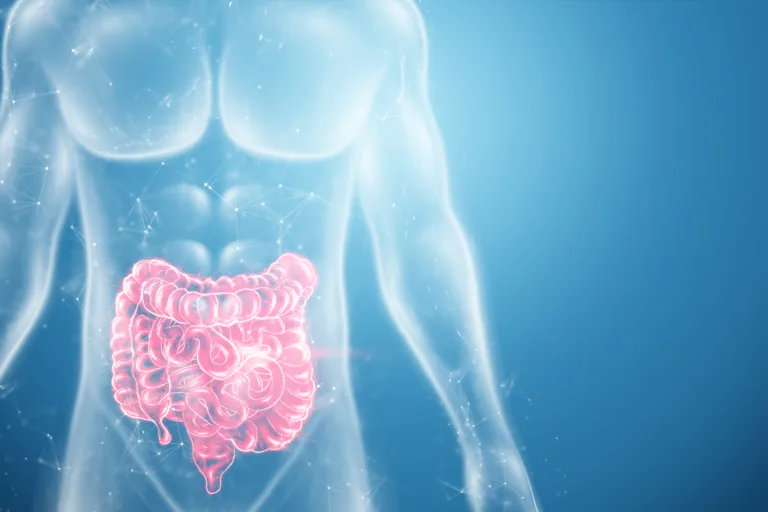
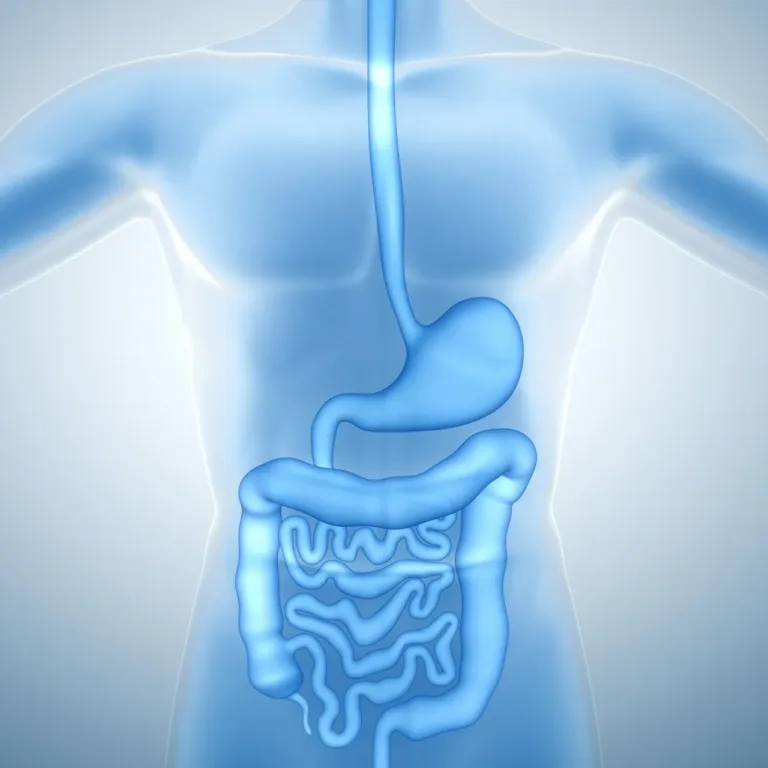
Q: What is the digestive system?
A: The digestive system is a series of organs that work together to break down food into nutrients that the body can absorb and use. It includes the mouth, oesophagus, stomach, small intestine, colon, rectum, and anus.
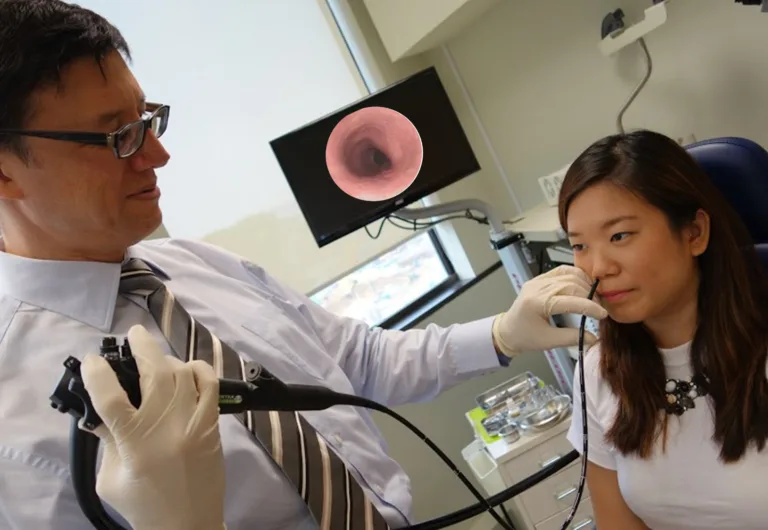
Q: What is endoscopy?
A: Endoscopy is a medical procedure that uses a thin, flexible tube with a camera and light on the end to examine the inside of the digestive system. It can diagnose and treat various conditions, including ulcers, polyps, and cancers.
Q: What is a colonoscopy?
A: A colonoscopy is a medical procedure that uses a flexible tube with a camera and light on the end to examine the inside of the colon. It can be used to screen for colon cancer, as well as to diagnose and treat a variety of conditions, including polyps and inflammatory bowel disease.
Q: What causes abdominal pain?
A: Abdominal pain can be caused by various factors, including infections, inflammation, injury, and structural abnormalities. It can also be a symptom of underlying medical conditions, such as appendicitis, gallstones, and peptic ulcer disease.
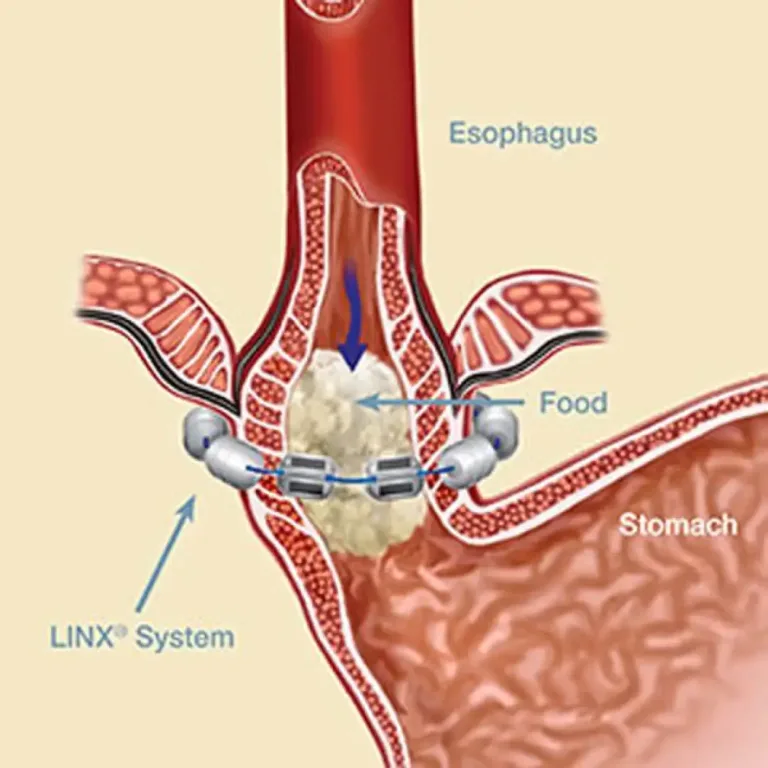
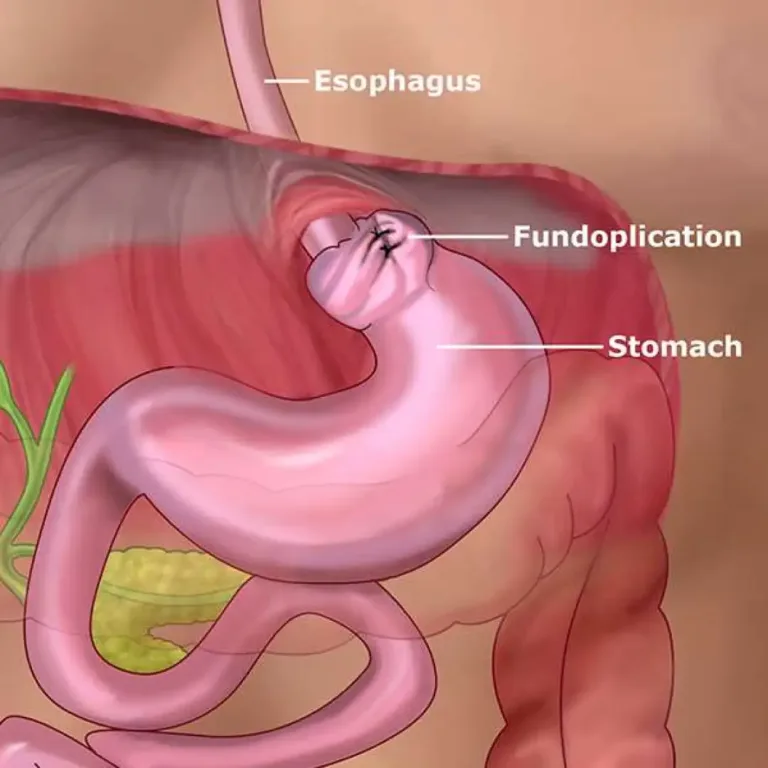
Q: What is reflux?
A: Reflux is when stomach acid flows back into the oesophagus, causing symptoms such as heartburn and regurgitation. A common condition can be managed with lifestyle changes and medications.
Q: What is an ulcer?
A: An ulcer is a sore or lesion that forms in the lining of the digestive system, typically in the stomach or duodenum. It can be caused by various factors, including infections, medications, and stress.
Q: What is inflammatory bowel disease (IBD)?
A: Inflammatory bowel disease (IBD) is a group of chronic conditions that cause inflammation in the digestive system, including Crohn’s disease and ulcerative colitis. Symptoms can include abdominal pain, diarrhoea, and weight loss.
Q: What is liver disease?
A: Liver disease refers to any condition that affects the function or structure of the liver. It can be caused by various factors, including viruses, alcohol use, and certain medications. Symptoms can include fatigue, jaundice, and abdominal pain.