What is Postcholecystectomy syndrome?
Conditions
What is Postcholecystectomy syndrome?
Postcholecystectomy syndrome (PCS) refers to a group of symptoms that can occur after removal of the gallbladder (cholecystectomy). This can include abdominal pain, bloating, diarrhea, constipation, and reflux, among others. The exact cause of PCS is not well understood, but it is thought to be related to changes in the way bile is metabolized in the body after removal of the gallbladder. Some people may also experience changes in the gut microbiome after cholecystectomy, which may contribute to symptoms of PCS. Treatment options for PCS can vary and may include changes to diet and lifestyle, medications to manage specific symptoms, and in some cases, additional surgeries.
Schedule an appointment
Related Articles
Gastroenterology
Understanding theFaecal calprotectin test
Faecal calprotectin results provide an objective...
Gastroenterology
Understanding the Faecal Occult Blood Test
A faecal occult blood test (FOBT) is a simple,...
Gastroenterology
TIF: A New Non-Surgical Option for GERD
For those suffering from chronic acid reflux...
Gastroenterology
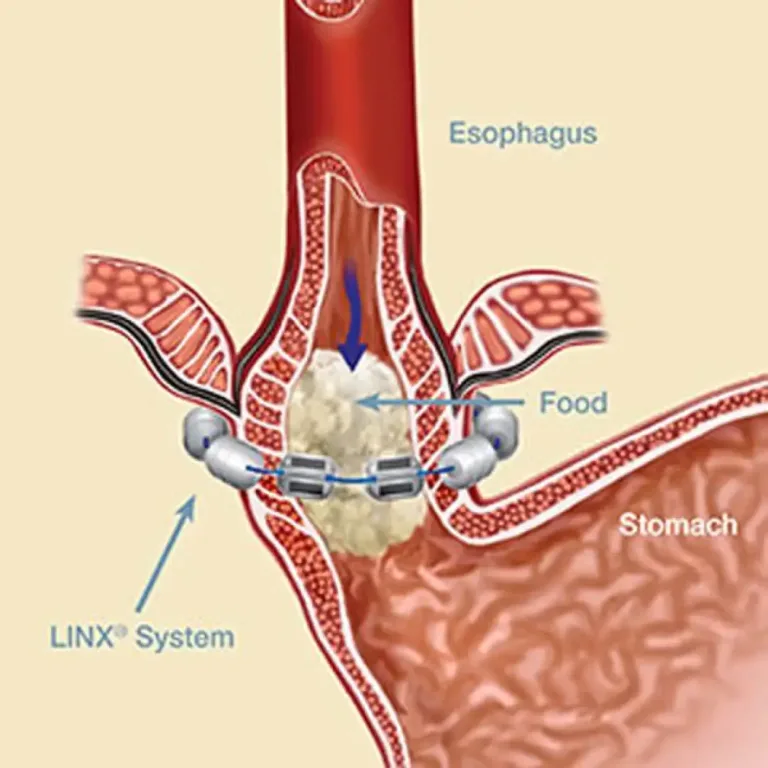
LINX Procedure: Minimally Invasive Relief for Reflux
Offering relief by reinforcing...
Gastroenterology
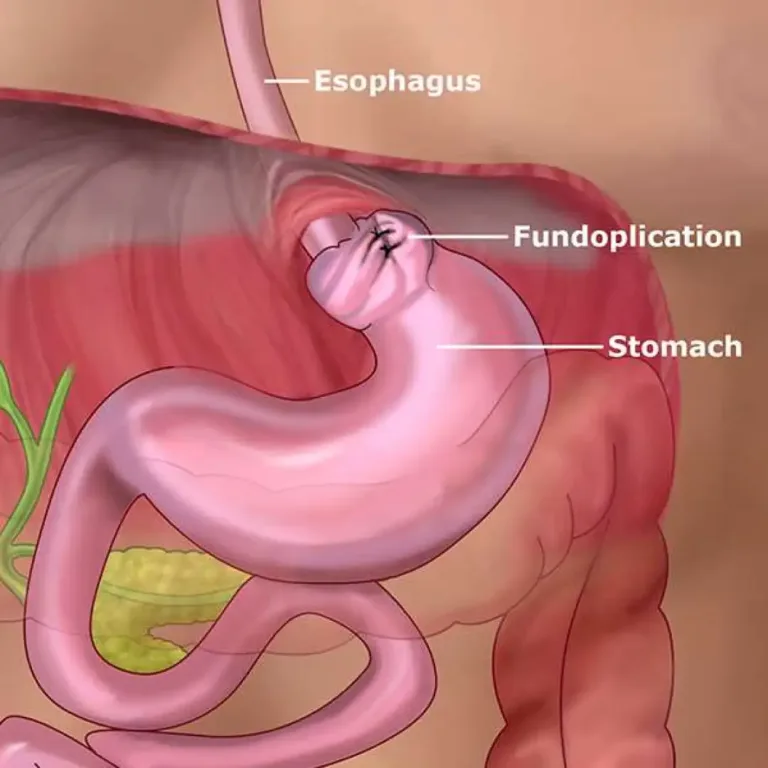
Nissen Fundoplication: A Surgical Solution for Reflux Disease
Nissen fundoplication,...
Gastroenterology
What is Gastroparesis
Gastroparesis, delayed gastric emptying, and issues with stomach...
What is Postcholecystectomy syndrome? Read More »